Sleep bruxism and perceived stress: assessment using salivary cortisol levels, a biomarker of stress
DOI:
https://doi.org/10.23921/amp.2023v7i2.00072Keywords:
Jaw muscle hyperactivity, Perceived stress, Salivary cortisol, Sleep bruxism, Stress biomarker, Teeth grindingAbstract
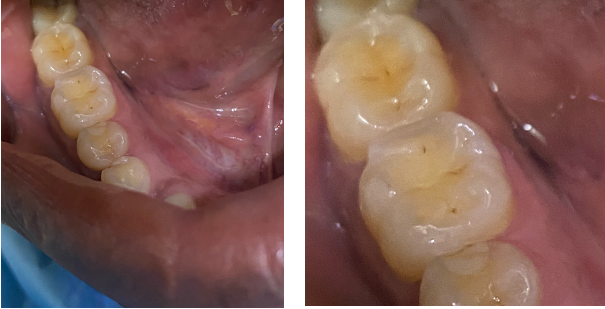
Sleep bruxism (SB) corresponds to physiologically based manducatory muscle reactions, with no identifiable neuropathic cause, in relation to anxiety disorders, respiratory disorders or behavioral "tocs". The aim of this study was to assess the relationship between SB and perceived stress by measuring salivary cortisol levels. The study included 61 consenting adult participants: 31 for the study group (bruxers) and 30 for the control group (no bruxers). The diagnosis of BS was made using a standard bruxism assessment questionnaire defined by the American Academy of Sleep Medicine (AASM). The preliminary diagnosis was confirmed by clinical assessment according to AASM criteria. The BRUXi index, a tool proposed by Orthlieb, was used to determine the intensity of bruxism. Perceived stress was measured using the Perceived Stress Scale questionnaire. Unstimulated whole saliva was collected and morning salivary cortisol levels were determined by ELISA. Non-parametric statistical methods were used to analyze the data. The bruxers (study group) had significantly high levels of mean salivary cortisol (12.3±4.2 ng/mL or 34.5±14.6 nmol/L) than the non-bruxers (control group) (5.3±1.2 ng/mL or 14.5±4.6 nmol/L) (p<0.001). The elevated salivary cortisol level was positively associated with perceived stress and SB (p<0.0001) in the study group. These results suggest that bruxing activity is associated with higher levels of perceived psychological stress and salivary cortisol. Despite the absence of polysomnographic recording for the diagnosis of SB, a positive correlation between SB and salivary cortisol levels was observed in bruxers.
Downloads
References
American Academy of Sleep Medicine. International Classification of Sleep Disorders, 3rd ed.; American Academy of Sleep Medicine: Darien, IL, USA, 2014.
Manfredini D, Winocur E, Guarda-Nardini L, Paesani D, Lobbezoo F. Epidemiology of bruxism in adults: a systematic review of the literature. J Orofac Pain. 2013;27(2):99-110.
Yap AU, Chua AP. Sleep bruxism: Current knowledge and contemporary management. J Conserv Dent. 2016;19(5):383-389.
Safari A, Jowkar Z, Farzin M. Evaluation of the relationship between bruxism and premature occlusal contacts. J Contemp Dent Pract. 2013;14(4):616-621.
Ommerborn MA, Giraki M, Schneider C, Fuck LM, Zimmer S, Franz M, Raab WH, Schaefer R. Clinical significance of sleep bruxism on several occlusal and functional parameters. Cranio. 2010;28(4):238-248.
Kato T, Montplaisir JY, Guitard F, Sessle BJ, Lund JP, Lavigne GJ. Evidence that experimentally induced sleep bruxism is a consequence of transient arousal. J Dent Res. 2003;82(4):284-288.
Kato T, Rompré P, Montplaisir JY, Sessle BJ, Lavigne GJ. Sleep bruxism: an oromotor activity secondary to micro-arousal. J Dent Res. 2001;80(10):1940-1944.
Macaluso GM, Guerra P, Di Giovanni G, Boselli M, Parrino L, Terzano MG. Sleep bruxism is a disorder related to periodic arousals during sleep. J Dent Res. 1998;77(4):565-573.
Melo G, Dutra KL, Rodrigues Filho R, Ortega AOL, Porporatti AL, Dick B, Flores-Mir C, De Luca Canto G. Association between psychotropic medications and presence of sleep bruxism: A systematic review. J Oral Rehabil. 2018;45(7):545-554.
Jorgi?-Srdjak K, Ivezi? S, Ceki?-Arambasin A, Bosnjak A. Bruxism and psychobiological model of personality. Coll Antropol. 1998;22 Suppl:205-212.
Kampe T, Edman G, Bader G, Tagdae T, Karlsson S. Personality traits in a group of subjects with long-standing bruxing behaviour. J Oral Rehabil. 1997;24(8):588-593.
Abe Y, Suganuma T, Ishii M, Yamamoto G, Gunji T, Clark GT, Tachikawa T, Kiuchi Y, Igarashi Y, Baba K. Association of genetic, psychological and behavioral factors with sleep bruxism in a Japanese population. J Sleep Res. 2012;21(3):289-296.
Manfredini D, Lobbezoo F. Role of psychosocial factors in the etiology of bruxism. J Orofac Pain. 2009;23(2):153-166.
Nakata A, Takahashi M, Ikeda T, Hojou M, Araki S. Perceived psychosocial job stress and sleep bruxism among male and female workers. Community Dent Oral Epidemiol. 2008;36(3):201-209.
Abekura H, Tsuboi M, Okura T, Kagawa K, Sadamori S, Akagawa Y. Association between sleep bruxism and stress sensitivity in an experimental psychological stress task. Biomed Res. 2011;32(6):395-399.
Y?ld?r?m B, K?rarslan Karagoz O, Tekeli Simsek A, Koca C, Cicek MF. Associations between self-reported bruxism, sleep quality, and psychological status among dental students in Turkey. Cranio. 2024;42(1):63-68.
Fluera?u MI, Bocsan IC, Buduru S, Pop RM, Vesa SC, Zaharia A, Negucioiu M, Iacob SM. The correlation between sleep bruxism, salivary cortisol, and psychological status in young, Caucasian healthy adults. Cranio. 2021;39(3):218-224.
Yaribeygi H, Panahi Y, Sahraei H, Johnston TP, Sahebkar A. The impact of stress on body function: A review. EXCLI J. 2017;16:1057-1072.
Herman JP, McKlveen JM, Ghosal S, Kopp B, Wulsin A, Makinson R, Scheimann J, Myers B. Regulation of the hypothalamic-pituitary-adrenocortical stress response. Compr Physiol. 2016;6(2):603-621.
Levine A, Zagoory-Sharon O, Feldman R, Lewis JG, Weller A. Measuring cortisol in human psychobiological studies. Physiol Behav. 2007;90(1):43-53.
Clow A, Thorn L, Evans P, Hucklebridge F. The awakening cortisol response: methodological issues and significance. Stress. 2004;7(1):29-37.
Levartovsky S, Msarwa S, Reiter S, Eli I, Winocur E, Sarig R. The association between emotional stress, sleep, and awake bruxism among dental students: a sex comparison. J Clin Med. 2021;11(1):10.
Pierce CJ, Chrisman K, Bennett ME, Close JM. Stress, anticipatory stress, and psychologic measures related to sleep bruxism. J Orofac Pain. 1995;9(1):51-56.
Orthlieb JD, Duminil G. Diagnostic: identifier le bruxeur [Diagnostic: identify patient with bruxism]. In: Espace ID France, editor. Le bruxisme, tout simplement [Bruxism, simply]. Paris: Duminil G, Orthlieb JD, eds; 2015:75-89.
Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385-396.
Carvalho AL, Cury AA, Garcia RC. Prevalence of bruxism and emotional stress and the association between them in Brazilian police officers. Braz Oral Res. 2008;22(1):31-35.
Valiente López M, van Selms MK, van der Zaag J, Hamburger HL, Lobbezoo F. Do sleep hygiene measures and progressive muscle relaxation influence sleep bruxism? Report of a randomised controlled trial. J Oral Rehabil. 2015;42(4):259-265.
Montero J, Gómez-Polo C. Personality traits and dental anxiety in self-reported bruxism. A cross-sectional study. J Dent. 2017;65:45-50.
Lobbezoo F, Ahlberg J, Glaros AG, Kato T, Koyano K, Lavigne GJ, de Leeuw R, Manfredini D, Svensson P, Winocur E. Bruxism defined and graded: an international consensus. J Oral Rehabil. 2013;40(1):2-4.
Casett E, Réus JC, Stuginski-Barbosa J, Porporatti AL, Carra MC, Peres MA, de Luca Canto G, Manfredini D. Validity of different tools to assess sleep bruxism: a meta-analysis. J Oral Rehabil. 2017;44(9):722-734.
Cavallo P, Carpinelli L, Savarese G. Perceived stress and bruxism in university students. BMC Res Notes. 2016;9(1):514.
Karakoulaki S, Tortopidis D, Andreadis D, Koidis P. Relationship between sleep bruxism and stress determined by saliva biomarkers. Int J Prosthodont. 2015;28(5):467-474.
Makino M, Masaki C, Tomoeda K, Kharouf E, Nakamoto T, Hosokawa R. The relationship between sleep bruxism behavior and salivary stress biomarker level. Int J Prosthodont. 2009;22(1):43-48.
Amato JN, Tuon RA, Castelo PM, Gavião MB, Barbosa TdeS. Assessment of sleep bruxism, orthodontic treatment need, orofacial dysfunctions and salivary biomarkers in asthmatic children. Arch Oral Biol. 2015;60(5):698-705.
Polmann H, Réus JC, Massignan C, Serra-Negra JM, Dick BD, Flores-Mir C, Lavigne GJ, De Luca Canto G. Association between sleep bruxism and stress symptoms in adults: A systematic review and meta-analysis. J Oral Rehabil. 2021;48(5):621-631.
Fritzen VM, Colonetti T, Cruz MVB, Ferraz SD, Ceretta L, Tuon L, DA Rosa MI, Ceretta RA. Levels of salivary cortisol in adults and children with bruxism diagnosis: a systematic review and meta-analysis. J Evid Based Dent Pract. 2022;22(1):101634.
Lavigne GJ, Kato T, Kolta A, Sessle BJ. Neurobiological mechanisms involved in sleep bruxism. Crit Rev Oral Biol Med. 2003;14(1):30-46.
Ohayon MM, Li KK, Guilleminault C. Risk factors for sleep bruxism in the general population. Chest. 2001;119(1):53-61.
Lavigne GJ, Khoury S, Abe S, Yamaguchi T, Raphael K. Bruxism physiology and pathology: an overview for clinicians. J Oral Rehabil. 2008;35(7):476-494.
Yamamoto T, Hirayama A. Effects of soft-diet feeding on synaptic density in the hippocampus and parietal cortex of senescence-accelerated mice. Brain Res. 2001;902(2):255-263.
Hori N, Lee MC, Sasaguri K, Ishii H, Kamei M, Kimoto K, Toyoda M, Sato S. Suppression of stress-induced nNOS expression in the rat hypothalamus by biting. J Dent Res. 2005;84(7):624-628.
Additional Files
Published
How to Cite
License
Copyright (c) 2023 Quench Academy of Medical Education and Research (QAMER)

This work is licensed under a Creative Commons Attribution 4.0 International License.
The authors warrants and represents that the submitted MANUSCRIPT is an original work and has not been published before in any form, and that it does not infringe upon any copyright or other right(s), that it does not contain infringing, libelous, obscene or other unlawful matter, that he/she is the sole and exclusive owner of the rights here-in conveyed to the Publisher, and that he/she has obtained the customary permission from the copyright owner or his legal representative whenever a text/passage from copyrighted material is quoted or a table or illustration from such material is used. The Author(s) will indemnify the Publisher for, and hold the Publisher harmless from any loss, expense or damage occasioned by any claim or suit by a third party for copyright infringement or arising out of any breach of the foregoing warranties as a result of publication of the Article. The Article shall be delivered to the Publisher free of copyright charges. In the event that the Article is not accepted and published by Publisher, this agreement becomes null and void.
Sherpa/Romeo publisher policy can be viewed at Annals of Medical Physiology - Sherpa/Romeo Policy
Plum X metrics
Article level metrics are shown here