Yoga vs physical activity: A comparative study of stress and sleep in young adults
Effect of yoga vs physical activity on stress and sleep quality
Revised : 2025-10-18
Accepted : 2025-10-20
Online : 2025-10-31
Print : 2025-10-31

Full text
Abstract
The high prevalence of stress and sleep disorders among medical students necessitates effective, non-pharmacological interventions. While both yogic breathing and physical activity are beneficial, their comparative efficacy on these specific outcomes remains unclear. This study aimed to compare the effects of a structured yogic breathing intervention and moderate-intensity physical activity on perceived stress levels and subjective sleep quality in healthy medical students. A prospective, randomized controlled trial was conducted with 170 participants allocated to either a Yogic Breathing Group (n=85) or a Physical Activity Group (n=85). The intervention lasted five weeks, with sessions conducted five days per week. The primary outcomes, psychological stress and sleep quality, were assessed using the Depression Anxiety Stress Scales (DASS-21) and the Pittsburgh Sleep Quality Index (PSQI), respectively, at baseline and post-intervention. Data were analyzed using paired t-tests and Analysis of co-variance. Both groups showed significant within-group improvements in stress (p<0.001). However, between-group analysis revealed that the Yogic Breathing group achieved a significantly greater reduction in DASS-21 scores compared to the Physical Activity group (mean Δ: -14.43 ± 6.21 vs. -3.69 ± 5.12; p<0.001). Conversely, the Physical Activity group demonstrated a significantly greater improvement in PSQI scores than the Yogic Breathing group (mean Δ: -0.96 ± 1.42 vs. -0.40 ± 1.05; p=0.012). Yogic breathing was superior for reducing perceived stress, whereas physical activity was more effective for enhancing sleep quality. The results indicate that both approaches complement each other rather than replace one another. Selecting the right approach should depend on the specific needs, helping to provide a more individualized plan for well-being.
Keywords: Medical students, Mental health, Physical activity, Sleep quality, Stress, Yogic breathing
How to cite: Manzoor A, Yograj S, Kapoor M, Singh M, Kaur T. Yoga vs physical activity: A comparative study of stress and sleep in young adults. Ann Med Physiol. 2025;8(1):1-6. doi: 10.23921/amp.2025v8i1.00075
Introduction
Stress is both a psychological perception of threat and a physiological activation of the body’s defense systems. Activation of the autonomic nervous system (ANS) and the hypothalamic–pituitary–adrenal (HPA) axis leads to the release of cortisol, adrenaline, and noradrenaline, preparing the body for “fight or flight” [1]. While adaptive in the short term, chronic stress results in dysregulation of autonomic and hormonal processes, predisposing individuals to cardiovascular disease, obesity, metabolic disorders, and impaired psychological well-being [1,2]. Stress also negatively affects higher-order brain functions, including memory, attention, and emotional regulation, thereby compromising resilience and overall health [3,4]. Among young adults, persistent stress has become highly prevalent due to academic, social, and financial pressures, highlighting the urgent need for effective non-pharmacological strategies [5,6]. Yoga and pranayama (yogic breathing practices) have been widely studied as accessible, evidence-based approaches for stress reduction. By modulating breathing rhythms, these practices stimulate vagal activity, shift autonomic balance towards parasympathetic dominance, and improve subjective well-being [7,8]. Similarly, regular aerobic physical activity enhances stress resilience by reducing sympathetic overdrive, lowering circulating stress hormones, improving sleep quality, and supporting mood and cognition through neurobiological pathways [9,10]. Both interventions are simple, cost-effective, and can be easily incorporated into daily routines, making them practical solutions for large populations such as students.
Although several studies have evaluated yoga and physical activity independently, most investigations focus on physiological measures such as heart rate variability (HRV), with limited emphasis on validated psychological and sleep-related outcomes. Few studies have directly compared yoga-based practices and physical activity in young adults using standardized tools like the Depression Anxiety Stress Scale (DASS-21) [11] and the Pittsburgh Sleep Quality Index (PSQI) [12]. Given the growing concern about stress-induced sleep disturbances in student communities, the combined evaluation of these outcomes is of particular importance. The present study addresses this gap by comparing the effects of structured Yogic Breathing and Physical Activity interventions on stress levels (DASS-21) [11] and sleep quality (PSQI) [12] in young adults.
Materials and methods
Participants and study design
This prospective, parallel-group, randomized controlled trial was conducted over a duration of 18 months. Ethical approval was obtained from the Institutional Ethics Committee, with ethical number of IEC/P-600/2024 and written informed consent was collected from all participants prior to enrollment. A total of 170 healthy medical students were recruited and randomized into two groups: the Yogic Breathing Group (n = 85) and the Physical Activity Group (n = 85). Participants were aged between 18 and 30 years, enrolled as full-time students, and medically stable with no known cardiovascular, neurological, psychiatric or endocrine disorders. Those engaged in regular yoga or structured physical activity in the last six months, substance users, or individuals with irregular sleep patterns or those with any self-reported or known diagnosis of a psychological disorder were excluded. Randomization was carried out using computer-generated block randomization (block size = 4), stratified by gender and baseline DASS-21 scores. Allocation concealment was ensured through sealed opaque envelopes.
Intervention protocols
Participants were allocated to one of the two intervention groups as outlined in Table 1. Each intervention was implemented over a period of five consecutive weeks, with sessions conducted five days per week under the supervision of qualified instructors. Each session lasted approximately 30 minutes [13,14], including additional time for rest and recovery to ensure participant comfort and optimal performance. For the Yogic Breathing Group, emphasis was placed on maintaining correct posture, breathing rhythm, and precise technique, while participants were also encouraged to engage in brief home practice supported by audio recordings to reinforce learning and enhance adherence. Similarly, participants in the Physical Activity Group were guided on exercise intensity, proper form, and progression, with the use of wearable devices for heart rate monitoring to maintain moderate-intensity activity levels. Both groups received weekly supervision throughout the study period to ensure intervention fidelity, participant compliance, and correct execution of techniques, thereby maintaining the rigor and reliability of the trial.
| Group | Intervention description | Intervention summary |
|---|---|---|
| Yogic Breathing Group (n =85) | Supervised yogic breathing sessions with 5-minute rest before and after |
Nadi Shodhana (alternate nostril breathing) Kapalabhati (forceful abdominal exhalations) Bhastrika (rapid diaphragmatic breathing) Sheetali (cooling breath with tongue roll) OM chanting |
| Physical Activity Group (n =85) | Moderate-intensity aerobic exercises of choice, matched in duration and frequency, at 60–80% of maximum heart rate (monitored) |
Walking Jogging Cycling Running Harward Step Dance routines |
Assessments and statistical analysis
Psychological stress and sleep quality were the primary outcomes. Stress was measured using the Depression, Anxiety, and Stress Scale (DASS-21) [11], and sleep quality was assessed using the Pittsburgh Sleep Quality Index (PSQI) [12]. Both scales were administered in English or Hindi by trained psychologists. Assessments were conducted at baseline (pre-intervention) and after five weeks (post-intervention), 48–72 hours following the last session [15]. Data were analyzed using SPSS v28. Within-group changes were assessed using paired t-tests, while between-group comparisons were made using Analysis of co-variance, adjusting for baseline values. Effect sizes with 95% confidence intervals were reported. A significance level of p < 0.05 was considered statistically significant.
Result
A total of 170 participants were randomized and completed the trial, with 85 participants in each groupBaseline demographic and anthropometric characteristics were comparable between the Yogic Breathing and Physical Activity groups, with no statistically significant differences (all p > 0.05), indicating successful randomization (Table 2).
| Parameter | Yogic Breathing group (n=85) | Physical Activity group (n=85) | p-value |
|---|---|---|---|
| Age (years) | 21.4 ± 1.7 | 21.6 ± 1.9 | 0.412 |
| Sex: Male/Female | 38 / 47 | 38 / 47 | 1.000 |
| Height (cm) | 165.8 ± 8.2 | 166.8 ± 8.8 | 0.387 |
| Weight (kg) | 61.9 ± 8.8 | 62.9 ± 9.4 | 0.476 |
| BMI (kg/m2) | 22.4 ± 2.0 | 22.8 ± 2.2 | 0.185 |
| Parameter | Pre-Yoga (Mean ± SD) | Post-Yoga (Mean ± SD) | Mean Difference (95% CI) | p-value |
|---|---|---|---|---|
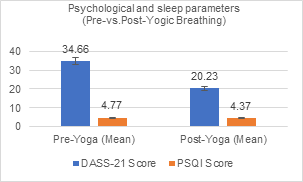
| DASS-21 score | 34.66 ± 6.21 | 20.23 ± 5.84 | -14.43 (-16.2, -12.6) | <0.001 |
| PSQI score | 4.77 ± 1.05 | 4.37 ± 0.98 | -0.40 (-0.85, 0.05) | 0.08 |
Yogic Breathing led to a significant reduction in DASS score (p < 0.001), indicating stress relief. PSQI improved slightly but was not statistically significant (p = 0.08).
| Parameter | Pre-PA (Mean) | Post-PA (Mean) | Mean Difference [95% CI] | p-value | Effect Size (Cohen's d) | Interpretation |
|---|---|---|---|---|---|---|
| DASS-21 score | 28.71 | 25.02 | -3.69 [-5.12, -2.26] | <0.001 | 0.57 (Medium) | Significant stress reduction |
| PSQI score | 3.96 | 3.00 | -0.96 [-1.42, -0.50] | <0.001 | 0.94 (Large) | Significant sleep improvement |
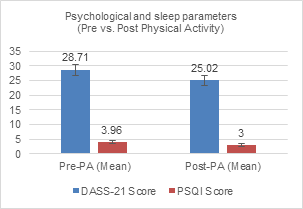
Significant improvements were seen in DASS score (p < 0.001) and PSQI (p < 0.001) with large effect sizes, indicating strong benefits for stress and sleep.
| Parameter | Yogic Breathing Group (Mean Δ ± SD) | Physical Activity Group (Mean Δ ± SD) | Between-Group p-value | Interpretation |
|---|---|---|---|---|
| DASS-21 score | -14.43 ± 6.21* | -3.69 ± 5.12* | <0.001 | Yogic Breathing reduced stress 3.9× more than Physical Activity (large effect). |
| PSQI score | -0.40 ± 1.05 | -0.96 ± 1.42* | 0.012 | Physical Activity improved sleep quality more than Yogic Breathing |
Discussion
The present study investigated the effects of Yoga-based breathing practices and moderate-intensity physical activity on psychological stress and sleep quality among medical students. Both groups demonstrated improvements in the Depression Anxiety Stress Scale (DASS-21) [11] and the Pittsburgh Sleep Quality Index (PSQI) [12] scores over the 5-week intervention period. However, the magnitude of improvement was greater for specific outcomes. Yogic breathing was significantly more effective than physical activity for reducing psychological stress, likely due to its direct modulation of autonomic nervous system function. Conversely, physical activity was superior to yoga for improving subjective sleep quality, potentially mediated through mechanisms of physical fatigue and circadian regulation. These findings are consistent with earlier evidence that mind-body interventions may offer additional psychological benefits compared to conventional physical activity alone.
Stress
Our findings highlight that participants in the Yogic Breathing group demonstrated a significantly greater reduction in DASS stress subscale scores compared to those in the Physical Activity group (Table 3, Table 5). While both interventions helped mitigate stress, Yoga showed superior effects (Figure 1 and Figure 2), likely due to its dual impact on both physiological relaxation and cognitive-emotional regulation. Previous studies have reported similar results, where yogic breathing enhanced parasympathetic activity, reduced cortisol secretion, and improved emotional stability in stressed populations (Streeter et al and Sharma et al) [16,17]. In contrast, physical activity has been shown to reduce stress through endorphin release and improved cardiovascular conditioning (Rebar et al) [18]. However, these benefits may not directly address the cognitive and emotional aspects of stress regulation to the same extent as Yogic Breathing. This explains why the Yogic Breathing group in our study achieved a more pronounced improvement in psychological stress compared to the Physical Activity group.
Sleep quality
A significant and unexpected finding of our study was the divergent effect on sleep quality. Contrary to our initial hypothesis, the physical activity group demonstrated a significant improvement in PSQI scores, while the change in the yoga group was minimal and not statistically significant (Figure 1 and Figure 2). This result clearly indicates that for subjective sleep quality, physical activity was the more effective intervention (Table 4, Table 5). This outcome can be explained on physiological grounds. Primarily, the nature of our yoga intervention is a key consideration. The protocol consisted exclusively of active, stimulating breathing exercises (e.g. Kapalabhati, Bhastrika) known for their energizing and sympathomimetic effects [7,8]. While excellent for enhancing alertness and reducing stress, these practices may be less conducive to sleep promotion than more calming, restorative yoga practices (e.g., Yoga Nidra, gentle asanas) which are traditionally associated with improving sleep [19,20]. The stimulating nature of our protocol, particularly if practiced later in the day, could have increased physiological arousal in some participants, thereby counteracting sleep-promoting effects. Furthermore, physical activity is well-established to improve sleep through mechanisms of physiological fatigue, thermoregulation, and circadian entrainment [21]. The tangible sense of physical tiredness induced by moderate-intensity exercise likely contributed to the participants perception of deeper, more restorative sleep, as captured by the self-reported PSQI. This study underscores that not all yoga practices are equal; the specific modality must be carefully matched to the desired health outcome. For sleep disturbances in a young adult population, physical activity or potentially a more restorative yoga style may be preferable to an active breathing-focused regimen.
Clinical significance
The clinical implications of these findings are nuanced and highly relevant for medical students, who are vulnerable to high levels of stress and sleep disturbances. Our results suggest that intervention programs should be tailored to the primary complaint. For students seeking primarily stress reduction, a short, daily yoga breathing practice is a highly effective and efficient tool. Conversely, for those whose primary concern is poor sleep, promoting regular moderate-intensity physical activity may be the more directly beneficial strategy. because chronic stress and poor sleep are known to impair memory, concentration, and overall academic performance (Lo et al.) [22]. Our finding challenges the assumption of a one-size-fits-all approach and demonstrates that these interventions are complementary rather than interchangeable. Wellness initiatives can therefore be optimized by offering both modalities and guiding students toward the practice that best addresses their individual needs. Given the minimal resource requirements and adaptability of both yoga breathing and physical activity, they can be easily incorporated into medical curricula and student support systems to provide a practical, holistic framework for managing well-being.
Limitations
This study utilized a specific protocol of active yogic breathing exercises, which may limit the generalizability of the results to other yoga practices that include more physical postures or restorative elements. Future research could explore the effects of different yoga styles. Additionally. Finally, qualitative feedback regarding participants’ experiences was not collected, which might have provided deeper insight into the perceived benefits of the interventions.
Conclusion
Both interventions provided benefits, but for distinct outcomes. Yogic Breathing was significantly more effective than physical activity for reducing psychological stress. Conversely, Physical Activity was superior to Yogic Breathing for improving subjective sleep quality. The results indicate that both approaches complement each other rather than replace one another. Selecting the right approach should depend on the specific needs, helping to provide a more individualized plan for well-being.
References
- Sheikh S, Rostami A, Shahbazi A, Abdollahi Nezhad F, Khazai O, Arbabisarjou A. Clinical effectiveness of guided breathing exercises in reducing anxiety, stress, and depression in COVID-19 patients. Sci Rep. 2024;14(1):26620. [Crossref] [Pubmed]
- Biggs A, Brough P. Stress and Coping Theory. In: Liamputtong P (eds). Handbook of Concepts in Health, Health Behavior and Environmental Health. Singapore: Springer; 2025:1-23. [Crossref]
- McEwen BS. Neurobiological and systemic effects of chronic stress. Chronic Stress (Thousand Oaks). 2017;1:2470547017692328. [Crossref] [Pubmed]
- Schakel L, Veldhuijzen DS, Crompvoets PI, Bosch JA, Cohen S, van Middendorp H, Joosten SA, Ottenhoff THM, Visser LG, Evers AWM. Effectiveness of stress-reducing interventions on the response to challenges to the immune system: A meta-analytic review. Psychother Psychosom. 2019;88(5):274-286. [Crossref] [Pubmed]
- Arnsten AF. Stress signalling pathways that impair prefrontal cortex structure and function. Nat Rev Neurosci. 2009;10(6):410-422. [Crossref] [Pubmed]
- Duman RS, Aghajanian GK, Sanacora G, Krystal JH. Synaptic plasticity and depression: new insights from stress and rapid-acting antidepressants. Nat Med. 2016;22(3):238-249. [Crossref] [Pubmed]
- Kavitha N, Pal P, Pal GK, Bharadwaj B, Nanda N. Effects of slow breathing exercises on cardiac autonomic functions in anxiety disorder-A randomised control trial. Ann Neurosci. 2024:09727531241266094. [Crossref] [Pubmed]
- Kuppusamy M, Kamaldeen D, Pitani R, Amaldas J, Ramasamy P, Shanmugam P, Vijayakumar V. Effects of yoga breathing practice on heart rate variability in healthy adolescents: a randomized controlled trial. Integr Med Res. 2020;9(1):28-32. [Crossref] [Pubmed]
- Lin LL, Chen YJ, Lin TY, Weng TC. Effects of resistance training intensity on heart rate variability at rest and in response to orthostasis in middle-aged and older adults. Int J Environ Res Public Health. 2022;19(17):10579. [Crossref] [Pubmed]
- Bellón JÁ, Conejo-Cerón S, Sánchez-Calderón A, Rodríguez-Martín B, Bellón D, Rodríguez-Sánchez E, Mendive JM, Ara I, Moreno-Peral P. Effectiveness of exercise-based interventions in reducing depressive symptoms in people without clinical depression: systematic review and meta-analysis of randomised controlled trials. Br J Psychiatry. 2021;219(5):578-587. [Crossref] [Pubmed]
- Lovibond SH, Lovibond PF. Manual for the Depression Anxiety Stress Scales. 2nd ed. Sydney: Psychology Foundation of Australia; 1995. ISBN: 9780733414237
- Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193-213. [Crossref] [Pubmed]
- World Health Organization. Global recommendations on physical activity for health. Geneva: WHO; 2010. ISBN: 9789241599979. Available from: https://www.who.int/publications/i/item/9789241599979
- American Heart Association. American Heart Association recommendations for physical activity in adults. Dallas (TX): American Heart Association (AHA); 2024. Available from: https://www.heart.org/en/healthy-living/fitness/fitness-basics/aha-recs-for-physical-activity-in-adults
- Staniszewski M, Tkaczyk J, Kęska A, Zybko P, Mróz A. Effect of rest duration between sets on fatigue and recovery after short intense plyometric exercise. Sci Rep. 2024;14(1):15080. [Crossref] [Pubmed]
- Streeter CC, Gerbarg PL, Saper RB, Ciraulo DA, Brown RP. Effects of yoga on the autonomic nervous system, gamma-aminobutyric-acid, and allostasis in epilepsy, depression, and post-traumatic stress disorder. Med Hypotheses. 2012;78(5):571-579. [Crossref] [Pubmed]
- Sharma M. Yoga as an alternative and complementary approach for stress management: a systematic review. J Evid Based Complementary Altern Med. 2014;19(1):59-67. [Crossref] [Pubmed]
- Rebar AL, Stanton R, Geard D, Short C, Duncan MJ, Vandelanotte C. A meta-meta-analysis of the effect of physical activity on depression and anxiety in non-clinical adult populations. Health Psychol Rev. 2015;9(3):366-378. [Crossref] [Pubmed]
- Hariprasad VR, Sivakumar PT, Koparde V, Varambally S, Thirthalli J, Varghese M, Basavaraddi IV, Gangadhar BN. Effects of yoga intervention on sleep and quality-of-life in elderly: A randomized controlled trial. Indian J Psychiatry. 2013;55(Suppl 3):S364-S368. [Crossref] [Pubmed]
- Nagendra RP, Maruthai N, Kutty BM. Meditation and its regulatory role on sleep. Front Neurol. 2012;3:54. [Crossref] [Pubmed]
- Kredlow MA, Capozzoli MC, Hearon BA, Calkins AW, Otto MW. The effects of physical activity on sleep: a meta-analytic review. J Behav Med. 2015;38(3):427-449. [Crossref] [Pubmed]
- Lo JC, Ong JL, Leong RL, Gooley JJ, Chee MW. Cognitive performance, sleepiness, and mood in partially sleep deprived adolescents: The need for sleep study. Sleep. 2016;39(3):687-698. [Crossref] [Pubmed]

