Sleep bruxism and perceived stress: assessment using salivary cortisol levels, a biomarker of stress
Salivary cortisol level and sleep bruxism
Revised : 2023-12-27
Accepted : 2023-12-31
Online : 2023-12-31
Print : 2023-12-31

Full text
Abstract
Sleep bruxism (SB) corresponds to physiologically based manducatory muscle reactions, with no identifiable neuropathic cause, in relation to anxiety disorders, respiratory disorders or behavioral “tocs”. The aim of this study was to assess the relationship between SB and perceived stress by measuring salivary cortisol levels. The study included 61 consenting adult participants: 31 for the study group (bruxers) and 30 for the control group (no bruxers). The diagnosis of BS was made using a standard bruxism assessment questionnaire defined by the American Academy of Sleep Medicine (AASM). The preliminary diagnosis was confirmed by clinical assessment according to AASM criteria. The BRUXi index, a tool proposed by Orthlieb, was used to determine the intensity of bruxism. Perceived stress was measured using the Perceived Stress Scale questionnaire. Unstimulated whole saliva was collected and morning salivary cortisol levels were determined by ELISA. Non-parametric statistical methods were used to analyze the data. The bruxers (study group) had significantly high levels of mean salivary cortisol (12.3±4.2 ng/mL or 34.5±14.6 nmol/L) than the non-bruxers (control group) (5.3±1.2 ng/mL or 14.5±4.6 nmol/L) (p<0.001). The elevated salivary cortisol level was positively associated with perceived stress and SB (p<0.0001) in the study group. These results suggest that bruxing activity is associated with higher levels of perceived psychological stress and salivary cortisol. Despite the absence of polysomnographic recording for the diagnosis of SB, a positive correlation between SB and salivary cortisol levels was observed in bruxers.
Keywords: Jaw muscle hyperactivity, Perceived stress, Salivary cortisol, Sleep bruxism, Stress biomarker, Teeth grinding
How to cite: Lecor PA, Dieng S, Soumboundou S, Seck A, Sall OH, Guirassy ML. Sleep bruxism and perceived stress: assessment using salivary cortisol levels, a biomarker of stress. Ann Med Physiol. 2023;7(2):8-14. doi: 10.23921/amp.2023v7i2.00072
Introduction
Sleep bruxism (SB) is defined by the American Academy of Sleep Medicine as a “repetitive jaw muscle activity characterized by the clenching or grinding of teeth and/or bracing or thrusting of the mandible” [1]. Sleep bruxism corresponds to physiologically based manducatory muscle reactions, with no identifiable neuropathic cause, in relation to stress and anxiety disorders, respiratory disorders or behavioral “tocs” [1]. Bruxism is a non-functional activity or a parafunctional habit. It has been classified according to many criteria, but the one most used in clinical practice differentiates between awake bruxism and sleep bruxism [1]. SB can lead to tooth wear or abrasion, hypermobility of the teeth, hypersensitivity of the teeth, hypertrophy of the masticatory muscles, pain in the masticatory muscles and temporomandibular disorders [2,3]. The etiology of bruxism is not well defined. Various etiological factors have been investigated, including occlusal interference and malocclusion [4,5], transient episodes of sleep arousal [6,7,8], psychotropic medication [9], personality characters [10,11], psychosocial factors [12,13,14] and psychological stress [15,16,17]. The term stress covers all the biological changes in an organism subjected to a stimulus capable of disrupting its homeostasis [18]. The stress reaction involves behavioral, biological and biochemical changes. It mainly activates the sympathetic nervous system, immediately and fleetingly, and the corticotropic axis, slightly delayed but more permanent [18]. Behavioral, biological and biochemical markers are used to assess stress, the latter being the most reliable [18]. Cortisol is a steroid hormone that is released in response to physical or psychological stress. The hypothalamus–pituitary–adrenal (HPA) axis is a regulatory system of the organism that connects the central nervous system (CNS) with the hormonal system; one of the end products, cortisol, helps the organism adapt to increased demands after challenge and maintain homeostasis [19]. While in blood both bound and free cortisol can be measured, only free cortisol is measured in saliva [20]. The awakening cortisol response is a discrete and dynamic part of the circadian cortisol secretory cycle. Its main role and importance for health has yet to be fully elucidated, however early evidence suggests that it may be physiologically significant [21]. Periods of stress, which are increasingly common in modern life, are often cited as factors responsible for bruxism. Bruxism could therefore be defined as a "modern" disease. Questioning the patient may reveal that the clenching and grinding accompany stressful events in everyday life, such as conflictual, professional or social, emotional or sexual problems. Studies on the relationship between stress and SB are contradictory. Some find that psychosocial factors and perceived stress are risk factors for SB [15,16,17]. Contrary to these results, two other studies have shown that there is no relationship between the degree of SB and self-reported stress [22,23].
The aim of this study was to assess the relationship between SB and perceived stress by measuring salivary cortisol levels (a biomarker of stress).
Material and methods
Study design
The study included 61 consenting adult participants: 30 for the control group (no bruxers) and 31 for the study group (bruxers). Participants were recruited between January 2021 and June 2022. The study was carried out at the periodontology clinic of the Institute of Odontology and Stomatology of the Cheikh Anta Diop University of Dakar for the recruitment of patients and the collection of saliva samples. Salivary cortisol was measured in the biochemistry laboratory of the Dalal Jaam Hospital.
Inclusion criteria
The study group were the patients who were diagnosed as positive for sleep bruxism aged between 18 and 65, in good general health and who had given their consent to take part in the study. The control group differed from the cases only in the absence of sleep bruxism. They came from the same target population, were aged between 18 and 60, in good general health and had given their consent to participate in the study. The control group was matched to the study group regarding age and sex.
The following were excluded from the study: patients with bruxism who had been treated for more than ten years for this condition, mentally retarded patients, patients using psychotropic drugs, patients with extensive prosthetic restorations, patients with severe neuromuscular diseases, primary malocclusions, patients taking drugs that alter the activity of the neuromuscular system, patients with existing conditions affecting cortisol levels, such as adrenal gland insufficiency, pregnant women on oral contraceptives, individuals with xerostomia and patients who had refused to take part in the study.
The study was approved by the Ethics Committee of the Faculty of Medicine, Pharmacy and Odonto-stomatology at Cheikh Anta Diop University in Dakar, Senegal.
Diagnosis of sleep bruxism
The primary diagnosis of SB was made using a standard bruxism assessment questionnaire defined by the American Academy of Sleep Medicine (AASM) [1]. The questions asked were as follows:
- Has anyone told you that you grind your teeth at night?
- Do your teeth, gums or jaw muscles hurt when you wake up?
- Has anyone heard you grinding your teeth at night?
- Is your jaw always tired or painful when you wake up in the morning?
- Do your teeth or gums always hurt when you wake up in the morning?
- Do you feel pain in your temples when you wake up in the morning?
The preliminary diagnosis was confirmed by clinical assessment according to AASM criteria [1].
- The presence of regular or frequent tooth grinding sounds occurring during sleep.
- The presence of one or more of the following clinical signs:
- Abnormal tooth wear consistent with above reports of tooth grinding during sleep.
- Transient morning jaw muscle pain or fatigue; and/or temporal headache; and/or jaw locking upon awakening consistent with above reports of tooth grinding during sleep.
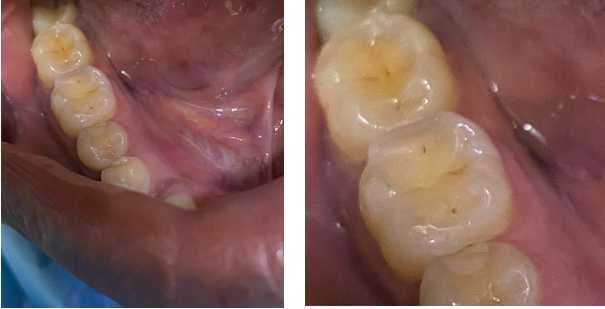
The BRUXi index, a tool proposed by Orthlieb and Duminil was used to determine the intensity of bruxism [24]. The BRUXi index is a score obtained from elements collected during the interview and clinical examination. The value of the index is obtained by adding the BRUXiq score (score obtained via the self-questionnaire) to the BRUXiex score (score obtained by collecting information in the clinical assessment). BRUXi = BRUXiq + BRUXiex. The intensity of sleep bruxism was defined as follows: low bruxism = BRUXi<20; moderate bruxism: 20<BRUXi<30 (Figure 1) and severe bruxism: BRUXi≥30 (Figure 2).

Questionnaire of stress
Perceived Stress Scale Questionnaire 14 (PSS-14): the level of emotional stress was measured using the PSS, developed by Cohen et al., 1983 [25]. The questionnaire consists of 14 items and examines stressful feelings and thoughts experienced by the respondent over the previous month. The respondent was asked to rate the frequency at which he/she experienced such feelings or thoughts on a scale of four ranging from “never” to “very often” (supplementary file), with a resulting total score ranging between 0 and 56 (a higher score indicated a higher level of emotional stress). PSS-14 scores ranging 0–18 was considered low perceived stress, 19–29 was considered moderate perceived stress and 30–56 was considered high perceived stress.
Assessment of salivary cortisol level
Saliva samples were taken in the morning between 7 and 8 A.M. All patients were asked not to eat and drink for 30 minutes before the sample collection. They were asked to rinse for 30 seconds with distilled water. Unstimulated whole saliva was collected by the spitting method in a sterile microcentrifuge tube. The collected saliva was stored in a refrigerator at -80°C. The stored saliva samples were subjected to an enzyme-linked immunosorbent assay (ELISA) test to detect salivary cortisol levels. On the day of the test, the saliva samples were prepared by centrifugation at 7000 rpm for 10 minutes to eliminate interference from glycoproteins. Once conditioned, the samples were used for analysis. Salivary cortisol was measured using a salivary cortisol enzyme-linked immunosorbent assay kit, in accordance with the manufacturer's instructions. The enzyme-linked immunosorbent reaction indicating cortisol level was measured by optical density which was read at 450 nm in a multimode plate reader. After collecting the data, results were tabulated, statistically analyzed, and compared. The normal reference value is 1.1-8.0 ng/mL or 3.1-22.2 nmol/L.
Statistical Analyses
The statistical analyses were performed using the SPSS (v20.0, Chicago, IL, USA) software. An analysis of variance (ANOVA) or t-test were used to determine significant mean differences and Pearson’s correlation for relationships among the variables. The non-parametric Mann-Whitney test was used to compare means in two groups (study and control) if the data did not follow normal distribution. In the study the correlation between the bruxism score and the stress score was assessed using Spearman's rho test. A level of p ≤ 0.05 was considered statistically significant.
Results
In the control group, 9 men and 21 women were enrolled, aged between 22 and 66 with an average age of 33.4 ± 8.4 years. In the study group, 11 men and 20 women were enrolled, aged between 20 and 69 with an average age of 35±19.5 years.
On questioning (BRUXiq) followed by clinical examination (BRUXiex), 21 patients (67.74%) suffered severe bruxism (BRUXi≥30), 9 patients (29.03%) moderate bruxism (20<BRUXi<30) and 1 patient (3.23%) low bruxism (BRUXi<20).
Comparing the study group with the control group, the results showed that the average score on the PSS-14 questionnaire was significantly higher for the study group than for the control group (p<0.001). There was a statistically significant difference between the study group and the control group with regard to the level of stress on the PSS-14 questionnaire: low, moderate and high (p<0.05) (Table 1). A detailed comparison of the results showed that the study group had significantly higher scores (49.39% versus 6.67% than the control group) (Table 1).
| Perceived stress scale (PSS-14) | Group | P-value | ||
|---|---|---|---|---|
| Control | Study | |||
| Average score (Mean±SD) | 19.62±7.64 | 33.12±11.24 | <0.001 | |
| Stress level | Low (n (%)) | 17 (56.67%) | 4 (12.9%) | <0.05 |
| Moderate (n (%)) | 11 (36.67%) | 12 (38.71%) | ||
| High (n (%)) | 2 (6.66%) | 15 (48.39%) | ||
| Total | 30 (100%) | 31 (100%) | ||
In the study group, a positive correlation was found between the perceived stress level (PSS-14 score) and the intensity of bruxism (the correlation coefficient was 0.433, p<0.01) (Table 2). In other words, the higher the PSS-14 score, the higher the intensity of bruxism (BRUXi index).
| BRUXi index | Stress level | |||
|---|---|---|---|---|
| Low (n (%)) | Moderate (n (%)) | High (n (%)) | Total (n (%)) | |
| *Statistically significant p value | ||||
| Severe bruxism (BRUXi≥30) | 1 (3.23) | 5 (16.12) | 15 (48.39) | 21 (67.74) |
| Moderate bruxism (20<BRUXi<30) | 2 (6.45) | 7 (22.58) | 0 (0) | 9 (29.03) |
| Low bruxism (BRUXi<20) | 1 (3.23) | 0 (0) | 0 (0) | 1 (3.23) |
| Total | 4 (12.90) | 12 (38.71) | 15 (48.39) | 31 (100) |
| Comparison* | Correlation coefficient r= 0.433, p<0.01 | |||
The bruxers (study group) had high levels of salivary cortisol (mean level = 12.3±4.2 ng/mL or 34.5±14.6 nmol/L; normal reference value = 1.1-8.0 ng/mL or 3.1-22.2 nmol/L). For the non-bruxers (control group), salivary cortisol levels were 5.3±1.2 ng/mL or 14.5±4.6 nmol/L. Comparison of salivary cortisol levels between the study group and the control group showed that the mean salivary cortisol score of the study group was significantly higher than that of the control group (p<0.001) (Figure 3).
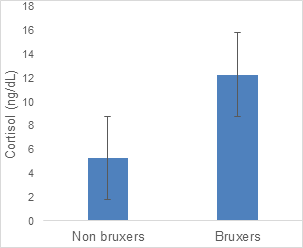
The elevated salivary cortisol level was positively associated with perceived stress and SB (p<0.0001) in the study group. However, in the control group, the salivary cortisol level was not statistically significant associated with perceived stress (p=0.34) (Table 3). However, there was no statistically significant association between the intensity of bruxism (BRUXi index) and the level of salivary cortisol (p = 0.401).
| Perceived stress scale (PSS-14) | Salivary cortisol level (ng/mL±SD or nmol/L±SD) | |
|---|---|---|
| Control group | Study group | |
| Average score | 5.3±1.2 or 14.5±4.6 | 12.3±4.2 or 34.5±14.6 |
| P-value* | 0.34 | <0.0001 |
Discussion
The present study assessed the relationship between SB and perceived stress using salivary cortisol levels, a biomarker of stress in patients with and without SB.
In our study, the subjects in the control group were aged between 22 and 66 years, with an average age of 33.4 ± 8.4 years. The subjects in the study group were aged between 20 and 69 years, with an average age of 35±19.5 years. Studies report varying mean ages: Carvalho et al (23.7 years) [26], Valiente et al (39.9 years) [27], Montero et al (43.7 years) [28]. Adult bruxism decreases with age and is more prevalent in people under 50 years [2].
Concerning the intensity of bruxism, 21 patients (67.74%) suffered from severe bruxism (BRUXi≥30), 9 patients (29.03%) moderate bruxism (20<BRUXi<30) and 1 patient (3.23%) mild bruxism (BRUXi<20). To quantify the intensity of bruxism, we used the BRUXi index of Orthlieb et al, which is a score obtained from elements collected during the interview (questionnaire) and clinical examination [24]. This method is used by some authors [29,30]. However, polysomnography remains the gold standard for the diagnosis of bruxism in the context of research projects [29,30], but it is not available to all researchers, and in dental practices, the most widely used method remains that based on clinical assessment. Orthlieb et al recommend combining assessment questionnaires with clinical examination for a more accurate diagnosis of bruxism [24]. Other very reliable means can also be used to quantify the intensity of bruxism namely electromyography (EMG) and polysomnography [29,30]. However, these tests are expensive, take a long time to analyze and need to be carried out in a specialized location or using portable devices. This limits their use in clinical practice.
Comparing the control group with the study group, the results showed that the mean score of the PSS-14 questionnaire was significantly higher for the study group than for the control group (p<0.001). The study group had a significantly higher frequency of perceived stress (49.39% versus 6.67%) than the control group. Furthermore, in the study group, a positive correlation was found between the level of perceived stress and the intensity of bruxism (r = 0.433, p<0.01). Our results are similar to those of other studies which consider that perceived stress is a risk factor for bruxism [15,16,17]. Questionnaires administered to patients with bruxism generally reveal stressful events in their daily lives, such as conflictual, professional, social, emotional or sexual problems. However, studies on the relationship between perceived stress and SB are contradictory. Studies have shown that there is no relationship between the degree of SB and self-reported stress [22,23,31]. Thus, the use of a recognized biological marker of stress such as salivary cortisol levels offer greater reliability to our results.
The main result of this study was that salivary cortisol levels were significantly higher than the normal reference values in the study group cortisol (mean level = 12.3±4.2 ng/mL or 34.5±14.6 nmol/L; normal reference value = 1.1-8.0 ng/mL or 3.1-22.2 nmol/L). In contrast, control subjects had normal salivary cortisol levels (mean level = 5.3±1.2 ng/mL or 14.5±4.6 nmol/L; normal reference value = 1.1-8.0 ng/mL or 3.1-22.2 nmol/L). The literature converges on a multifactorial etiology of SB, but there is a hypothesis that stress is the main factor in the development of sleep bruxism [15,16,17]. Currently, the collection of saliva samples to determine the presence of cortisol, a biomarker of stress, is widely used, mainly because it is a non-invasive, safe and simple method [32,33,34]. The study by Fluerașu et al analyzed the association between SB, salivary cortisol and psychological state in healthy adults. Sixty healthy students (with or without bruxism) were included in the study. Salivary cortisol was measured using the ELISA technique. Subjects with SB showed a general state characterized by anxiety or stress compared with subjects without SB. They also showed a depressive or anxious attitude induced by work compared with healthy individuals. Salivary cortisol levels were higher in SB subjects and in women and were correlated with the subjects' general anxiety, but not with a work-induced psychological state. They concluded that SB is correlated with general and work-induced psychological changes. Salivary cortisol could be a non-invasive marker for assessing the severity of SB [17]. Another study by Karakoulaki et al involving 55 volunteers (20 men, 25 women) aged between 25 and 55, whose diagnosis of bruxism was first clinical and then confirmed by EMG (but at home, using a single-use portable device) showed that in subjects with SB, perceived stress was significantly higher than in those without the condition. Salivary cortisol levels were significantly higher in the SB group, but salivary α-amylase levels showed no significant difference between the SB and non-SB groups [32].
However, few studies were found in a systematic review using salivary cortisol levels to assess the relationship between SB and perceived stress [35]. Most studies have used questionnaires to assess the relationship between SB and perceived stress. Our study used a reliable biological marker of stress. This systematic review showed that SB patients had higher levels of some self-reported stress symptoms, assessed using questionnaires, with a mean difference of 4.59 (95% CI: 0.26-8.92). Biomarkers such as epinephrine, norepinephrine, cortisol, adrenaline, dopamine, noradrenaline and prolidase enzyme levels also showed a positive association with SB. Although some associations were identified between probable SB and self-reported stress symptoms and biomarkers of stress in adults, these results should be interpreted with caution, as the quality of the evidence was found to be very low. These results suggest that further and better designed studies are needed to clarify the link between SB and stress [35]. A recent systematic review showed that in a total of six primary studies, involving 854 participants, analysis of cortisol levels showed a significant difference in favor of the control group of 1.10 (95% CI: 0.68-1.53), showing that patients with bruxism have higher salivary cortisol levels [36].
Daily events have an impact on the nocturnal activity of the masseter muscles. Any daytime stress would lead to nocturnal muscle tension/hyperactivity [37]. The existence of a genuine causal link between stress and bruxism [38] has been demonstrated by analyzing the influence of these neurotransmitters on manducatory muscle activity. Several central nervous system structures, such as the vegetative (sympathetic) nervous system [37], the brainstem [37,39] and the limbic system [40], are involved in generating rhythmic jaw movements and modulating muscle tone during sleep. The anatomical structures involved in the stress mechanism are the sympathetic nervous system and the limbic system, via the hypothalamic-pituitary-adrenal (HPA) axis [41]. Stimulation of these structures during a stressful episode triggers the secretion of stress hormones, which are catecholamines (adrenaline, noradrenaline and dopamine, produced by the adrenal glands), Corticotropin Releasing Hormone (CRH, produced by the hypothalamus), cortisol (produced by the adrenal glands, under the influence of CRH) and serotonin [6,41].
Conclusion
Our results suggest that SB activity is associated with higher levels of perceived psychological stress and salivary cortisol. Despite the absence of polysomnographic recording for the diagnosis of SB, a positive correlation between SB and salivary cortisol levels was observed in bruxers. These results should encourage further studies involving larger samples and using, in addition to questionnaires and clinical assessment, other methods such as electromyography of the masticatory muscles, polysomnography and functional magnetic resonance imaging (fMRI), which should make it possible to study a possible cause-and-effect relationship between perceived stress, salivary cortisol levels and SB.
References
- American Academy of Sleep Medicine. International Classification of Sleep Disorders, 3rd ed.; American Academy of Sleep Medicine: Darien, IL, USA, 2014.
- Manfredini D, Winocur E, Guarda-Nardini L, Paesani D, Lobbezoo F. Epidemiology of bruxism in adults: a systematic review of the literature. J Orofac Pain. 2013 Spring;27(2):99-110. [Crossref] [Pubmed]
- Yap AU, Chua AP. Sleep bruxism: Current knowledge and contemporary management. J Conserv Dent. 2016 Sep-Oct;19(5):383-9. [Crossref] [Pubmed] [Pubmed Central]
- Safari A, Jowkar Z, Farzin M. Evaluation of the relationship between bruxism and premature occlusal contacts. J Contemp Dent Pract. 2013 Jul 1;14(4):616-21. [Crossref] [Pubmed]
- Ommerborn MA, Giraki M, Schneider C, Fuck LM, Zimmer S, Franz M, Raab WH, Schaefer R. Clinical significance of sleep bruxism on several occlusal and functional parameters. Cranio. 2010 Oct;28(4):238-48. [Pubmed]
- Kato T, Montplaisir JY, Guitard F, Sessle BJ, Lund JP, Lavigne GJ. Evidence that experimentally induced sleep bruxism is a consequence of transient arousal. J Dent Res. 2003 Apr;82(4):284-8. [Crossref] [Pubmed]
- Kato T, Rompré P, Montplaisir JY, Sessle BJ, Lavigne GJ. Sleep bruxism: an oromotor activity secondary to micro-arousal. J Dent Res. 2001 Oct;80(10):1940-4. [Crossref] [Pubmed]
- Macaluso GM, Guerra P, Di Giovanni G, Boselli M, Parrino L, Terzano MG. Sleep bruxism is a disorder related to periodic arousals during sleep. J Dent Res. 1998 Apr;77(4):565-73. [Crossref] [Pubmed]
- Melo G, Dutra KL, Rodrigues Filho R, Ortega AOL, Porporatti AL, Dick B, Flores-Mir C, De Luca Canto G. Association between psychotropic medications and presence of sleep bruxism: A systematic review. J Oral Rehabil. 2018 Jul;45(7):545-554. [Crossref] [Pubmed] Epub 2018 May 3.
- Jorgić-Srdjak K, Ivezić S, Cekić-Arambasin A, Bosnjak A. Bruxism and psychobiological model of personality. Coll Antropol. 1998 Dec;22 Suppl:205-12. [Pubmed]
- Kampe T, Edman G, Bader G, Tagdae T, Karlsson S. Personality traits in a group of subjects with long-standing bruxing behaviour. J Oral Rehabil. 1997 Aug;24(8):588-93. [Crossref] [Pubmed]
- Abe Y, Suganuma T, Ishii M, Yamamoto G, Gunji T, Clark GT, Tachikawa T, Kiuchi Y, Igarashi Y, Baba K. Association of genetic, psychological and behavioral factors with sleep bruxism in a Japanese population. J Sleep Res. 2012 Jun;21(3):289-96. [Crossref] [Pubmed] Epub 2011 Oct 1.
- Manfredini D, Lobbezoo F. Role of psychosocial factors in the etiology of bruxism. J Orofac Pain. 2009 Spring;23(2):153-66. [Pubmed]
- Nakata A, Takahashi M, Ikeda T, Hojou M, Araki S. Perceived psychosocial job stress and sleep bruxism among male and female workers. Community Dent Oral Epidemiol. 2008 Jun;36(3):201-9. [Crossref] [Pubmed]
- Abekura H, Tsuboi M, Okura T, Kagawa K, Sadamori S, Akagawa Y. Association between sleep bruxism and stress sensitivity in an experimental psychological stress task. Biomed Res. 2011 Dec;32(6):395-9. [Crossref] [Pubmed]
- Yıldırım B, Kırarslan Karagoz O, Tekeli Simsek A, Koca C, Cicek MF. Associations between self-reported bruxism, sleep quality, and psychological status among dental students in Turkey. Cranio. 2024 Jan;42(1):63-68. [Crossref] [Pubmed] Epub 2021 Apr 1.
- Fluerașu MI, Bocsan IC, Buduru S, Pop RM, Vesa SC, Zaharia A, Negucioiu M, Iacob SM. The correlation between sleep bruxism, salivary cortisol, and psychological status in young, Caucasian healthy adults. Cranio. 2021 May;39(3):218-224. [Crossref] [Pubmed] Epub 2019 May 27.
- Yaribeygi H, Panahi Y, Sahraei H, Johnston TP, Sahebkar A. The impact of stress on body function: A review. EXCLI J. 2017 Jul 21;16:1057-1072. [Crossref] [Pubmed] [Pubmed Central]
- Herman JP, McKlveen JM, Ghosal S, Kopp B, Wulsin A, Makinson R, Scheimann J, Myers B. Regulation of the Hypothalamic-Pituitary-Adrenocortical Stress Response. Compr Physiol. 2016 Mar 15;6(2):603-21. [Crossref] [Pubmed] [Pubmed Central]
- Levine A, Zagoory-Sharon O, Feldman R, Lewis JG, Weller A. Measuring cortisol in human psychobiological studies. Physiol Behav. 2007 Jan 30;90(1):43-53. [Crossref] [Pubmed] Epub 2006 Oct 19.
- Clow A, Thorn L, Evans P, Hucklebridge F. The awakening cortisol response: methodological issues and significance. Stress. 2004 Mar;7(1):29-37. [Crossref] [Pubmed]
- Levartovsky S, Msarwa S, Reiter S, Eli I, Winocur E, Sarig R. The Association between Emotional Stress, Sleep, and Awake Bruxism among Dental Students: A Sex Comparison. J Clin Med. 2021 Dec 21;11(1):10. [Crossref] [Pubmed] [Pubmed Central]
- Pierce CJ, Chrisman K, Bennett ME, Close JM. Stress, anticipatory stress, and psychologic measures related to sleep bruxism. J Orofac Pain. 1995 Winter;9(1):51-6. [Pubmed]
- Orthlieb JD, Duminil G. Diagnostic: identifier le bruxeur [Diagnostic: identify patient with bruxism]. In: Espace ID France, editor.Le bruxisme, tout simplement [Bruxism, simply]. Paris: Duminil G, Orthlieb JD, eds; 2015:75-89.
- Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983 Dec;24(4):385-96. [Pubmed]
- Carvalho AL, Cury AA, Garcia RC. Prevalence of bruxism and emotional stress and the association between them in Brazilian police officers. Braz Oral Res. 2008 Jan-Mar;22(1):31-5. [Crossref] [Pubmed]
- Valiente López M, van Selms MK, van der Zaag J, Hamburger HL, Lobbezoo F. Do sleep hygiene measures and progressive muscle relaxation influence sleep bruxism? Report of a randomised controlled trial. J Oral Rehabil. 2015 Apr;42(4):259-65. [Crossref] [Pubmed] Epub 2014 Nov 21.
- Montero J, Gómez-Polo C. Personality traits and dental anxiety in self-reported bruxism. A cross-sectional study. J Dent. 2017 Oct;65:45-50. [Crossref] [Pubmed] Epub 2017 Jul 3.
- Lobbezoo F, Ahlberg J, Glaros AG, Kato T, Koyano K, Lavigne GJ, de Leeuw R, Manfredini D, Svensson P, Winocur E. Bruxism defined and graded: an international consensus. J Oral Rehabil. 2013 Jan;40(1):2-4. [Crossref] [Pubmed] Epub 2012 Nov 4.
- Casett E, Réus JC, Stuginski-Barbosa J, Porporatti AL, Carra MC, Peres MA, de Luca Canto G, Manfredini D. Validity of different tools to assess sleep bruxism: a meta-analysis. J Oral Rehabil. 2017 Sep;44(9):722-734. [Crossref] [Pubmed] Epub 2017 Jun 5.
- Cavallo P, Carpinelli L, Savarese G. Perceived stress and bruxism in university students. BMC Res Notes. 2016 Dec 21;9(1):514. [Crossref] [Pubmed] [Pubmed Central]
- Karakoulaki S, Tortopidis D, Andreadis D, Koidis P. Relationship Between Sleep Bruxism and Stress Determined by Saliva Biomarkers. Int J Prosthodont. 2015 Sep-Oct;28(5):467-74. [Crossref] [Pubmed]
- Makino M, Masaki C, Tomoeda K, Kharouf E, Nakamoto T, Hosokawa R. The relationship between sleep bruxism behavior and salivary stress biomarker level. Int J Prosthodont. 2009 Jan-Feb;22(1):43-8. [Pubmed]
- Amato JN, Tuon RA, Castelo PM, Gavião MB, Barbosa Tde S. Assessment of sleep bruxism, orthodontic treatment need, orofacial dysfunctions and salivary biomarkers in asthmatic children. Arch Oral Biol. 2015 May;60(5):698-705. [Crossref] [Pubmed] Epub 2015 Feb 20.
- Polmann H, Réus JC, Massignan C, Serra-Negra JM, Dick BD, Flores-Mir C, Lavigne GJ, De Luca Canto G. Association between sleep bruxism and stress symptoms in adults: A systematic review and meta-analysis. J Oral Rehabil. 2021 May;48(5):621-631. [Crossref] [Pubmed] Epub 2021 Jan 28.
- Fritzen VM, Colonetti T, Cruz MVB, Ferraz SD, Ceretta L, Tuon L, DA Rosa MI, Ceretta RA. Levels of salivary cortisol in adults and children with bruxism diagnosis: a systematic review and meta-analysis. J Evid Based Dent Pract. 2022 Mar;22(1):101634. [Crossref] [Pubmed] Epub 2021 Aug 30.
- Lavigne GJ, Kato T, Kolta A, Sessle BJ. Neurobiological mechanisms involved in sleep bruxism. Crit Rev Oral Biol Med. 2003;14(1):30-46. [Crossref] [Pubmed]
- Ohayon MM, Li KK, Guilleminault C. Risk factors for sleep bruxism in the general population. Chest. 2001 Jan;119(1):53-61. [Crossref] [Pubmed]
- Lavigne GJ, Khoury S, Abe S, Yamaguchi T, Raphael K. Bruxism physiology and pathology: an overview for clinicians. J Oral Rehabil. 2008 Jul;35(7):476-94. [Crossref] [Pubmed]
- Yamamoto T, Hirayama A. Effects of soft-diet feeding on synaptic density in the hippocampus and parietal cortex of senescence-accelerated mice. Brain Res. 2001 Jun 1;902(2):255-63. [Crossref] [Pubmed]
- Hori N, Lee MC, Sasaguri K, Ishii H, Kamei M, Kimoto K, Toyoda M, Sato S. Suppression of stress-induced nNOS expression in the rat hypothalamus by biting. J Dent Res. 2005 Jul;84(7):624-8. [Crossref] [Pubmed]

