Relationship between obesity, physical activity, sleeping hours and red blood cell parameters in adult Sudanese population
Effect of exercise and sleep hours on RBC parameters
Revised: 2019-05-21
Accepted: 2019-06-26
Online: 2019-06-28
Print: 2019-06-30

Full text
Abstract
Ideal body weight with proper physical activity and good sleep are essential parameters for good quality of life. This study is concerned with assessing the association of general obesity, physical activity and sleeping hours with hemoglobin (Hb) concentration and red blood cell (RBC) parameters in healthy adults in Sudan. In this cross sectional study, 1086 healthy adults between 20 and 60 years were included out of which 275 were males and 811 were females. A complete blood count (CBC) was performed for Hb, RBC count, PCV, MCH and MCHC using Sysmex KX-21 automated hematology analyzer. The median and 95 percentile (2.5th to 97.5th) range values for Hb and RBC count in underweight were 13.0 (Range: 9.6-16.7) g/dl and 4.6 (Range: 3.6-5.8) ×103/µL respectively, while Hb and RBC count in obese were 13.1 (Range: 10.4-17.0) g/dl and 4.6 (Range: 3.7-5.9) ×103/µL respectively, with no significant difference. The RBC count (p=0.004) and Hb (p≤0.001) were significantly high in physically active compared to physically inactive participants; whereas the hemoglobin concentration (p=0.047), red blood cells (p=0.007) and hematocrit (p≤0.001) values were significantly low in long-term sleep compared to normal sleeping hours. In conclusion, there were no significant differences in hemoglobin concentration, RBC count, PCV, MCH and MCHC between under weight, normal weight, overweight and obese persons. Increased physical activity was associated with higher Hb levels and RBC counts, while long-term sleep showed lower Hb and RBCs.
Keywords
Exercise, Obesity, Sleep, Sudan
Introduction
Enlarged adipose tissue increases the risk of diabetes, hypertension, cardiovascular disease and respiratory disorders. Furthermore, it effects iron status in the body [1]. Obesity is also associated with subclinical inflammation which might contribute to development of anemia. On the contrary, severe weight loss is associated with significant decrease in C-reactive protein (CRP) which is the main acute phase protein and a sensitive marker of systemic inflammation indicating that fat mass plays an important role in the production of CRP [2]. Several studies demonstrated that the anemia is directly associated with general obesity and physical inactivity [3,4,5].
It has been reported that exercise exerts physiological stress on the body that leads to hormonal, cellular and physical changes like raised blood pressure, body temperature and increase oxygen intake, which depends on number of factors such as the type and duration of exercise [6]. The effects of exercise and training on the hemopoietic system have been a hot topic in sports medicine. Many recent studies centered on hypothesis of sports anemia induced by endurance training. It is well documented that exercise training can stimulate erythropoiesis and increase red cell mass as well as plasma volume, resulting in increased blood volume [7,8,9,10]. Hematological parameters might be influenced by the type and intensity of the physical activity [11].
Sleep is defined as a state of reversible loss of consciousness [12]. Sleep is a biological process that is very much essential for optimal health and survival. It plays an important role in maintaining functions of brain, metabolism, immune system, hormonal and cardiovascular systems [13,14]. Good quality sleep can be described as sufficient sleep time and regularity with absence of any sleep disorders [15].
This study was concerned with evaluating the association of obesity, physical activity and sleep hours with hemoglobin concentration and RBC parameters in healthy adults in Sudan.
Materials and methods
Ethical approval was obtained from the Sudanese Federal Ministry of Health in Sudan (FMOH) (Reference number: 1-10-2016) and The National Ribat University.
This descriptive cross sectional study was done in Sudan during 2017-2018. 1086 adults were included (275 males and 811 females). Subjects with hematological disorders or chronic diseases like hypertension, diabetes mellitus, liver diseases, renal diseases, cardiac diseases, tuberculosis, asthma, thyroid disorders, or with recent acute diseases (Malaria, typhoid fever, etc.) were excluded. Any subject with recent history of surgery especially splenectomy were also excluded. All healthy Sudanese people between 20 and 60 years were included. All selected subjects answered a structured questionnaire containing personal, clinical and life style information. Written consent was taken from each participant.
Age in years (Date of birth), standing height in cm (without footwear) was recorded on a wall mounted measuring tape and weight in kg (without footwear) was recorded on weighing scale. Body mass index (BMI) in kg/m2 was calculated. Participants were then grouped into 4 categories: underweight, normal weight, overweight and obese based on BMI. 3 ml of venous blood was collected into K3-EDTA vacutainer and was analyzed using Sysmex KX-21 automated hematology analyzer.
Statistical analysis
Normality of continuous variable data was determined by using the Shapiro-Wilk test and normal Q-Q plot. The parametric continuous variables are presented as a mean±SD while non-parametric continuous variables are presented as a median (interpercentile range) and analyzed by Mann-Whitney U test. One-way, two-way analyses of variance (ANOVA) and Student t-test were applied for normally distributed continuous variables. While Mann-Whitney U test was used for non-pramatric continuos variables.
Firstly three tests were performed (skewness, kurtosis and the Kolmogorov Smirnov) to determine the normality of our data. The test results was significant (p<0.05). Therefore, we used non-parametic method to determine the reference range, the reference intervals was calculated by using lower and upper percentile limits with the 95% confidence intervals as the following: Lower percentile limit ws set to the 2.5th and upper percentile limit was set to 97.5th percentile.
Statistical tests were 2-sided, and p value less than 0.05 was considered significant. All statistical analyses were performed using the SPSS version 25 (IBM SPSS Inc., Chicago, USA).
Results
The mean age of the total 1086 participants was 25±9 years. The mean age slightly varied between genders: 28.6 years for males and 24.2 years for females. The mean height, weight and BMI were 162±50, 61±14 and 22.9±4.9 respectively. The red blood cell (RBC) count, hemoglobin (Hb) and hematocrit (HCT) and blood indices showed no significant differences with different body mass index categories (Table 1 and Table 2).
| Parameter | Under weight (N=207) | Normal (N=522) | Over weight (N=201) | Obese (N=85) | p value |
|---|---|---|---|---|---|
| Data presented as median (Interpercentile range) | |||||
| RBC count (x103/μL) | 4.6 (3.6-5.8) | 4.6 (3.7-5.9) | 4.6 (3.8-5.8) | 4.6 (3.7-5.9) | 0.384 |
| Hb (g/dl) | 13.0 (9.6-16.7) | 12.9 (9.3-17.0) | 12.9 (9.7-16.3) | 13.1 (10.4-17.0) | 0.558 |
| Parameter | Under weight (N=207) | Normal (N=522) | Over weight (N=201) | Obese (N=85) | p value |
|---|---|---|---|---|---|
| Data presented as median (Interpercentile range) | |||||
| HCT (%) | 39.5 (36.4-44.0) | 39.7 (36.4-44.1) | 38.8 (35.5-42.9) | 40.5 (36.7-45.4) | 0.205 |
| MCH (pg) | 28.7 (26.8-30.3) | 28.4 (26.3-30.0) | 28.3 (26.1-29.6) | 29.1 (26.5-30.5) | 0.071 |
| MCHC (%) | 32.6 (30.3-34.3) | 32.4 (30.8-34.2) | 32.9 (31.2-34.6) | 32.6 (31.1-34.7) | 0.366 |
Our result showed that, red blood cells and hemoglobin had significant positive correlation with height and weight (Table 3).
| Parameter | Height | Weight |
|---|---|---|
| **p value ≤ 0.001 | ||
| RBCs | 0.223** | 0.134** |
| Hb | 0.220** | 0.131** |
In context of physical activity, the mean height, weight and BMI in physically active individuals (Exercise group) were 195±22, 60±13 and 22.6±4.8 respectively, while in physically inactive group the mean of height was 164±66, weight and BMI were 61±14 and 22.8±4.9 respectively. There are no significant differences in weight, height and BMI between exercise and no exercise group (Table 4).
| Parameter | Exercise (N=491) | No exercise (N=523) | p value |
|---|---|---|---|
| Numbers represent mean±SD | |||
| Height (cm) | 195±22 | 164±66 | 0.761 |
| Weight (kg) | 60±13 | 61±14 | 0.482 |
| BMI (kg/m2) | 22.6±4.8 | 22.8±4.9 | 0.284 |
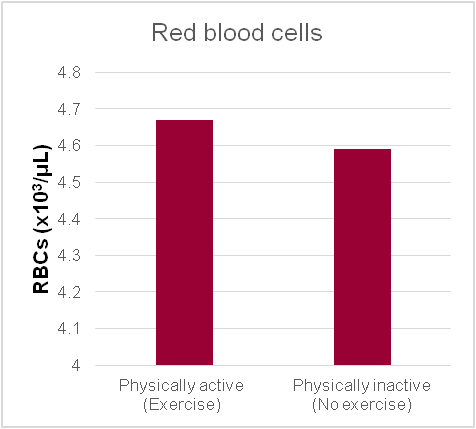
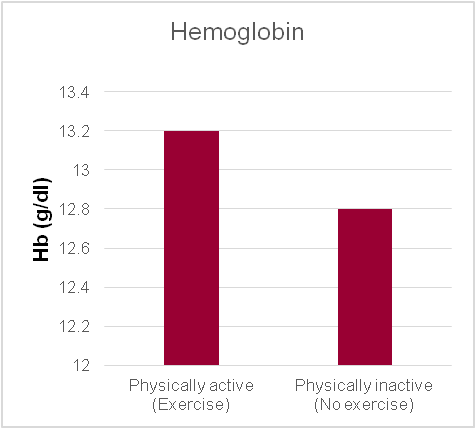
Our result showed significantly higher RBC count (p=0.004) and Hb (p≤0.001) in physically active individuals (Exercise group) compared with physically inactive (No exercise) group (Figure 1 and Figure 2).
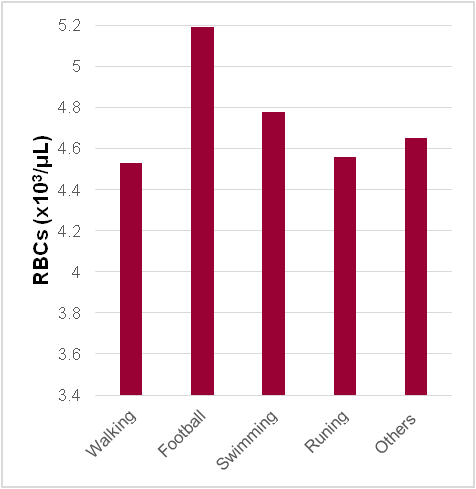
Our result showed football players had significantly higher hemoglobin (p≤0.001) and red blood cells levels (p≤0.001) compared with other type of physical activities (Table 5 and Figure 3).
| Parameter | n | Hb | p value |
|---|---|---|---|
| Numbers represent mean±SD | |||
| Walking | 249 | 12.9±1.9 | ≤0.001 |
| Football | 127 | 15.7±1.6 | |
| Swimming | 74 | 13.5±1.7 | |
| Running | 29 | 13.5±1.7 | |
| Others | 12 | 13.1±1.9 | |
Our results showed significant variation in weight and BMI with sleeping hours; short sleep duration is associated with more weight and BMI (Table 6).
| <6 hours | 6-8 hours | >8 hours | p value | |
|---|---|---|---|---|
| Numbers represent mean±SD | ||||
| Weight | 63±14 | 60±13 | 59±13 | 0.034 |
| BMI | 23.3±4.4 | 22.6±4.8 | 22.8±5.6 | 0.05 |
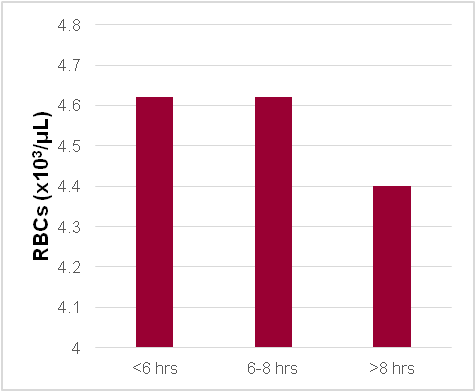
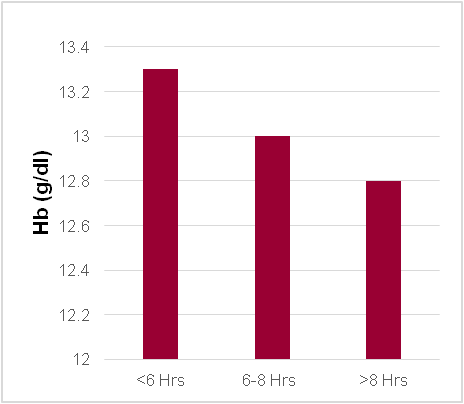
Our results showed that the hemoglobin concentration, red blood cells and hematocrit were significantly low in long-term sleep compared with normal sleeping hours (Table 7; Figure 4 and Figure 5).
| Parameter | <6 hours (n=195) | 6-8 hours (n=646) | >8 hours (n=89) | p value |
|---|---|---|---|---|
| Numbers represent median (interpercentile range) | ||||
| RBCs (×103/µL) | 4.62 (3.68-5.78) | 4.62 (3.73-5.87) | 4.40 (3.48-5.84) | 0.007 |
| Hb (g/dl) | 13.3 (9.3-16.6) | 13.0 (9.6-16.9) | 12.8 (9.5-15..2) | 0.047 |
| Hematocrit (%) | 38.9 (30.4-52.7) | 40.0 (31.2-54.2) | 37.1 (30.0-52.2) | <0.001 |
Discussion
Our study results showed that there is no or weak association between BMI, hemoglobin, hematocrit and red blood cells indices; this is in agreement with many previous studies [16,17,18]. On the other hand many researchers demonstrated that low BMI is one of the reasonable predictors of anemia [3,19]. Furthermore, one study observed that females with central obesity developed anemia less than normal weight women [4]. A study conducted in older Koreans reported that the advancing age, low BMI and the female gender are independent risk factors for anemia [20]. The possible explanation for this inverse association between high BMI and anemia might be well nutritional status of obese people with high intake of iron containing foods.
In our study we found that hemoglobin and red blood cells are significantly high in physically active participants. These findings agree with many studies that examined the effect of aerobic exercise (for 8 to 12 weeks) on the red blood cells and hemoglobin content and found significant increase in red blood cells and hemoglobin levels [21,22,23]. Exercise or training programs less than 8 weeks does not have significant change in red blood cells and hemoglobin level [8,24,25,26] while long training programs more the 12 weeks lead to decrease hemoglobin level [27,28]. Our result showed significant inverse association between BMI and sleep duration, this finding is in accordance with one study [29], other study reported that BMI was effected only by short sleep duration [30]. It is noteworthy that both short and long sleep duration increase chances of future body weight gain in adults [31]. The possible explanation for this finding might be the association of short sleep duration with disturbance in adipokinase secretion that lead to weight gain [32]. Short sleep duration obviously increases awake duration that increases frequency of eating which would add to the total calorie intake. It has also been suggested that daytime tiredness and fatigue in addition to changed eating patterns may result in less physical exercise, which in turn reduces the body’s total energy expenditure, and thereby increasing the risk of obesity [33].
Our results showed significant decrease in hemoglobin, red blood cells and hematocrit in long-term sleeping (>8 hours) compared with normal (6-8 hours) sleep duration. This supports the findings of another study which demonstrated high hemoglobin and red blood cells parameters in insomnia patient [34]. On the contrary, one study revealed that anemia was associated with short sleep duration in elderly (>50 years) persons [35]. Other study observed that, there is no significant difference in sleep duration between anemic and non-anemic individuals [36]. One of the possible mechanisms that might link sleep duration with anemia is increased plasma level of inflammatory markers such as C-reactive protein that appear to increase in long sleep duration [37].
Conclusion
There were no statistically significant differences in Hb, RBC count, hematocrit, MCH and MCHC between under weight, normal weight, overweight and obese persons. Increased physical activity was associated with higher Hb levels and RBC counts, while long-term sleep showed lower Hb and RBCs.
Source of funding
This study was funded by the National Ribat University, Sudan.
Acknowledgments
The authors would like to thank the study volunteers for their participation.
References
- Yanoff LB, Menzie CM, Denkinger B, Sebring NG, T McHugh T, Remaley AT, Yanovski. JA. Inflammation and iron deficiency in the hypoferremia of obesity. Int J Obes (Lond). 2007 Sep; 31(9):1412-9. [Pubmed] [Crossref]
- Chen SB, Lee YC, Ser KH, Chen JC, Chen SC, Hsieh HF, Lee WJ. Serum C-reactive protein and white blood cell count in morbidly obese surgical patients. Obes Surg. 2009 Apr; 19(4):461-6. [Pubmed] [Crossref]
- Ausk KJ, Ioannou GN. Is obesity associated with anemia of chronic disease? A population-based study. Obesity (Silver Spring) 2008 Oct; 16(10): 2356-61. [Pubmed] [Crossref]
- Qin Y, Melse-Boonstra A, Pan X, Yuan B, Dai Y, Zhao J, Zimmermann MB, Kok FJ, Zhou M, Shi Z. Anemia in relation to body mass index and waist circumference among Chinese women. Nutr J. 2013 Jan 11; 12:10. [Pubmed] [Crossref]
- Cepeda-Lopez AC, Osendarp SJ, Melse-Boonstra A, Aeberli I, Gonzalez-Salazar F, Feskens E, Villalpando S, Zimmermann MB. Sharply higher rates of iron deficiency in obese Mexican women and children are predicted by obesity-related inflammation rather than by differences in dietary iron intake. Am J ClinNutr. 2011 May; 93(5): 975-83. [Pubmed] [Crossref]
- Bhatti R, Shaikh DM. The effect of exercise on blood parameters. Pak J Physiol. 2007 Dec 31; 3(2).
- Convertino VA. Blood volume response to physical activity and inactivity. Am J Med Sci. 2007 Jul; 334(1):72-9. [Pubmed] [Crossref]
- Sawka MN, Convertino VA, Eichner ER, Schnieder SM, Young AJ. Blood volume: importance and adaptations to exercise training, environmental stresses, and trauma/sickness. Med Sci Sports Exerc. 2000 Feb; 32(2):332-48. [Pubmed]
- Schmidt W, Prommer N. Impact of alterations in total hemoglobin mass on VO2max. Exerc Sport Sci Rev. 2010 Apr; 38(2):68-75. [Pubmed] [Crossref]
- Convertino VA. Blood volume: its adaptation to endurance training. Med Sci Sports Exerc. 1991 Dec; 23(12):1338-48. [Pubmed]
- Bezci Ş, Kaya Y. The analyze of hematological parameters of elite women taekwondoers before and after training. Pamukkale J Sport Sci. 2010; 1(2):1-16.
- Kryger MH, Roth T, Dement WC, eds. Principles and Practice of Sleep Medicine. 4th ed. Philadelphia: W.B. Saunders Company; 2005.
- Consensus Conference Panel, Watson NF, Badr MS, Belenky G, Bliwise DL, Buxton OM, Buysse D, Dinges DF, Gangwisch J, Grandner MA, Kushida C, Malhotra RK, Martin JL, Patel SR, Quan SF, Tasali E. Joint Consensus Statement of the American Academy of Sleep Medicine and Sleep Research Society on the recommended amount of sleep for a healthy adult: Methodology and discussion. Sleep. 2015 Aug; 38(8):1161-83. [Pubmed] [Crossref]
- Institute of Medicine (US) Committee on Sleep Medicine and Research; Colten HR, Altevogt BM, eds. Sleep disorders and sleep deprivation: An unmet public health problem. Washington (DC): National Academies Press; 2006. [Pubmed]
- Watson NF, Badr MS, Belenky G, Bliwise DL, Buxton OM, Buysse D, Dinges DF, Gangwisch J, Grandner MA, Kushida C, Malhotra RK, Martin JL, Patel SR, Quan SF, Tasali E. Recommended amount of sleep for a healthy adult: A joint consensus statement of the American Academy of Sleep Medicine and Sleep Research Society. Sleep. 2015 Jun; 38(6):843-4. [Pubmed] [Crossref]
- Semba RD, Ricks MO, Ferrucci L, Xue QL, Guralnik JM, Fried LP. Low serum selenium is associated with anemia among older adults in the United States. Eur J Clin Nutr. 2009 Jan; 63(1): 93-9. [Pubmed] [Crossref]
- Ghadiri-Anari A, Nazemian N, Vahedian-Ardakani HA. Association of body mass index with hemoglobin concentration and iron parameters in Iranian population. ISRN Hematol. 2014 Feb; 2014:525312. [Pubmed] [Crossref]
- Acharya S, Patnaik M, Mishra SP, Panigrahi AK. Correlation of hemoglobin versus body mass index and body fat in young adult female medical students. Natl J Physiol Pharm Pharmacol. 2018 Oct; 8(10):1371-3. [Crossref]
- Zakai NA, Katz R, Hirsch C, Shlipak MG, Chaves PH, Newman AB, Cushman M. A prospective study of anemia status, hemoglobin concentration, and mortality in an elderly cohort: the Cardiovascular Health Study. Arch Intern Med. 2005 Oct; 165(19): 2214-20. [Pubmed] [Crossref]
- Choi CW, Lee J, Park KH, Yoon SY, Choi IK, Oh SC, Seo JH, Kim YH, Kim JS. Prevalence and characteristics of anemia in the elderly: cross-sectional study of three urban Korean population samples. Am J Hematol. 2004 Sep; 77 (1): 26-30. [Pubmed] [Crossref]
- Gallagher PM, Carrithers JA, Godard MP, Schulze KE, Trappe SW. Beta-hydroxy-beta-methylbutyrate ingestion, part II: effects on hematology, hepatic and renal function. Med Sci Sports Exerc. 2000 Dec; 32(12): 2116-9. [Pubmed]
- Sazvar A, Mohammadi M, Nazem F, Farahpour N. The effect of morning aerobic exercise on some hematological parameters in young, active males. Iranian Journal of Health and Physical activity. 2013; 4(1):23-8.
- Cengiz ŞŞ, Çinar V. The effect of 8-week core exercises on some hematological parameters in sedentary females. Turkish J Sci Res. 2014; 1(1): 1-5
- Mashiko T, Umeda T, Nakaji S, Sugawara K. Effects of exercise on the physical condition of college rugby players during summer training camp. Br J Sports Med. 2004 Apr; 38(2):186-90. [Pubmed] [Crossref]
- Yeh SH, Chuang H, Lin LW, Hsiao CY, Eng HL. Regular tai chi chuan exercise enhances functional mobility and CD4CD25 regulatory T cells. Br J Sports Med. 2006 Mar; 40(3):239-43. [Pubmed] [Crossref]
- Senturk UK, Yalcin O, Gunduz F, Kuru O, Meiselman HJ, Baskurt OK. Effect of antioxidant vitamin treatment on the time course of hematological and hemorheological alterations after an exhausting exercise episode in human subjects. J Appl Physiol (1985). 2005 Apr; 98(4):1272-9. [Pubmed] [Crossref]
- Fujitsuka S, Koike Y, Isozaki A, Nomura Y. Effect of 12 weeks of strenuous physical training on hematological changes. Mil Med. 2005 Jul; 170(7):590-4. [Pubmed] [Crossref]
- Schmidt W, Prommer N. Effects of various training modalities on blood volume. Scand J Med Sci Sports. 2008 Aug; 18 Suppl 1:57-69. [Pubmed] [Crossref]
- Meyer KA, Wall MM, Larson NI, Laska MN, Neumark-Sztainer D. Sleep duration and body mass index in a sample of young adults. Obesity (Silver Spring). 2012 Jun; 20(6): 1279-87. [Pubmed] [Crossref]
- Peltzer K, Pengpid S. Sleep duration, sleep quality, body mass index, and waist circumference among young adults from 24 low- and middle-income and two high-income countries. Int J Environ Res Public Health. 2017 May; 14(6):E566. [Pubmed] [Crossref]
- Chaput JP, Després JP, Bouchard C, Tremblay A. The association between sleep duration and weight gain in adults: a 6-year prospective study from the Quebec Family Study. Sleep. 2008 Apr; 31(4):517-23. [Pubmed] [Crossref]
- Taheri S, Lin L, Austin D, Young T, Mignot E. Short sleep duration is associated with reduced leptin, elevated ghrelin and increased body mass index. PLoS Med. 2004 Dec; 1(3):e62. [Pubmed] [Crossref]
- Taheri S. The link between short sleep duration and obesity: we should recommend more sleep to prevent obesity. Arch Dis Child. 2006 Nov; 91(11):881-4. [Pubmed] [Crossref]
- Johann AF, Hertenstein E, Kyle SD, Baglioni C, Feige B, Nissen C, McGinness AJ, Riemann D, Spiegelhalder K. Insomnia with objective short sleep duration is associated with longer duration of insomnia in the Freiburg Insomnia Cohort compared to insomnia with normal sleep duration, but not with hypertension. PLoS One. 2017 Jul 26; 12(7): e0180339. [Pubmed] [Crossref]
- Jackowska M, Kumari M, Steptoe A. Sleep and biomarkers in the English Longitudinal Study of Ageing: associations with C-reactive protein, fibrinogen, dehydroepiandrosterone sulfate and hemoglobin. Psychoneuroendocrinology. 2013 Sep; 38(9):1484-93. [Pubmed] [Crossref]
- Murat S, Ali U, Serdal K, Süleyman D, İlknur P, Mehmet S, Bahattin A, Tunahan U. Assessment of subjective sleep quality in iron deficiency anaemia. Afr Health Sci. 2015 Jun; 15(2): 621-7. [Pubmed] [Crossref]
- Meier-Ewert HK, Ridker PM, Rifai N, Regan MM, Price NJ, Dinges DF, Mullington JM. Effect of sleep loss on C-reactive protein, an inflammatory marker of cardiovascular risk. J Am Coll Cardiol. 2004 Feb 18; 43(4):678-83. [Pubmed] [Crossref]

