Electrocardiographic changes in patients with pre-eclampsia
ECG changes in pre-eclampsia
Department of Physiology,
Regional Institute of Medical Sciences,
Lamphelpat, Imphal-795004,
Manipur, India.
Department of Physiology,
Regional Institute of Medical Sciences,
Lamphelpat, Imphal-795004,
Manipur, India.
Professor, Department of Physiology,
Regional Institute of Medical Sciences,
Lamphelpat, Imphal-795004,
Manipur, India.
Department of Physiology,
Regional Institute of Medical Sciences,
Lamphelpat, Imphal-795004,
Manipur, India.
Revised: 2019-02-27
Accepted: 2019-03-07
Online: 2019-03-22
Print: 2019-03-31

Full text
Abstract
Pre-eclampsia is a hypertensive disorder of pregnancy that is associated with elevated maternal risk for cardiovascular disease. Electrocardiographic (ECG) changes in pre-eclampsia have been documented in some studies. Electrocardiography has recently emerged as a useful tool to evaluate cardiovascular complication during and after pregnancy. The present study was therefore undertaken to find out electrocardiographic changes in pre-eclamptic women, visiting Regional Institute of Medical Sciences, Manipur. The aim of this study was to determine the electrocardiographic changes in both pre-eclampsia and age matched normotensive pregnant women. In this study, 25 pregnant women (gestational age >20 weeks) with pre-eclampsia in the range of 18 to 45 years of age were recruited and compared with the equal number of age matched normotensive pregnant women. ECG parameters of pre-eclamptic women were compared with those of normotensive pregnant women. The data were then analyzed using SPSS software. Pre-eclamptic women showed significantly longer QRS (0.10±0.02 sec vs 0.09±0.05 sec), prolonged QT (0.401±0.03 sec vs 0.365±0.003sec) and QTc (457.73±37 msec vs 416.47± 25.4 msec) than control group. The study shows that electrocardiography can be used to evaluate cardiovascular risk in pre-eclamptic women.
Keywords
ECG, Pre-eclampsia, QRS, QTc, Sokolow-Lyon index
Introduction
Pre-eclampsia is known to be a leading cause of maternal and neonatal death worldwide. Pre-eclampsia is a pregnancy-specific multi-organ syndrome that effects 2% to 8% of pregnancy [1]. It is characterized by development of hypertension to the extent of 140/90 mm Hg or more with proteinuria after the 20th week of gestation in a previously normotensive and non-proteinuric patient [2]. The clinical features usually develop in the latter part of the third trimester i.e. close to term (near 38-40th weeks of gestation) and progress until delivery. This disorder is unique to human pregnancy in which numerous genetic, immunological and environmental factors interact [3]. Pre-eclampsia is associated with high maternal mortality and fetal complication. It is not only a short term risk but also has an increased maternal cardiovascular risk later on. It was hypothesized that abnormal perfusion of the uterine arteries and linked feedback mechanisms of the fetoplacental unit are associated with increased stress on the maternal heart which in turn effect maternal ventricular repolarization [4].
ECG changes in pre- eclampsia have been documented in some studies. ECG recently emerged as a useful tool to evaluate cardiovascular complications during and after pregnancy. Specifically, left atrial abnormalities detected by standard ECG are associated with a fourfold increased risk of hypertensive disorders during pregnancy [5]. While the physiological changes in the ECG during pregnancy have been documented, the pattern of ECG in hypertensive disorders of pregnancy has not yet adequately been studied in India. This has prompted the need of this study.
Materials and methods
This case control study was carried out in the Department of Physiology in collaboration with Department of Obstetrics & Gynecology, Regional Institute of Medical Sciences (RIMS), Imphal. The study was done with the approval of the Research Ethics Board, RIMS, Imphal (Ref No. A/206/REB-comm(SP)/RIMS/2015/140/8/2016) following ICMR guidelines and informed consent was taken from each subject. 25 pregnant women (gestational age >20 weeks) with pre-eclampsia in the range of 18 to 45 years of age were recruited as cases and compared with the controls of equal number of age matched normotensive pregnant women. Those with history of chronic hypertension, thyroid dysfunction, cardiovascular disease, diabetes mellitus, other systemic diseases and history of intake of any medication that might effect cardiovascular functions were excluded from the study. To avoid interference with the reliability of the electrocardiography test all subjects were asked to avoid all caffeine containing edible items (tea/coffee/chocolate) 4 hours prior to the test.
A portable electrocardiograph — Cardiart 108T/MK (BPL limited, India) was used to record ECG. ECG parameters used in the study included six study variables namely HR, P-wave, QRS-wave, PR-wave, QT-wave, QTc-wave and Sokolow-Lyon index. Sokolow-Lyon index is a criteria used to diagnose left ventricular hypertrophy via electrocardiography and is calculated as S in V1 + R in V5 or V6 (whichever is larger) ≥35 mm (≥7 large squares). Mean values of ECG parameters in both cases and controls were calculated and using independent-t test the ECG parameters of pre-eclamptic women were compared with those of normotensive pregnant women. The data were then analysed using SPSS software version 21 (IBM SPSS, Chicago, USA).
Results
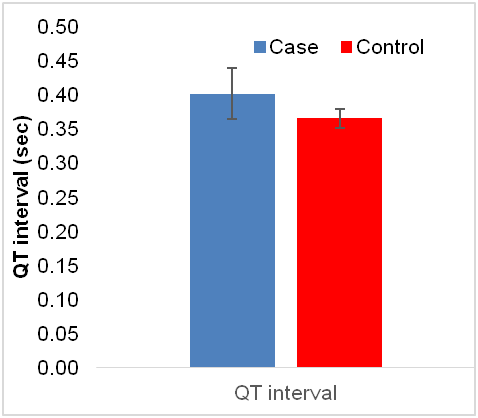
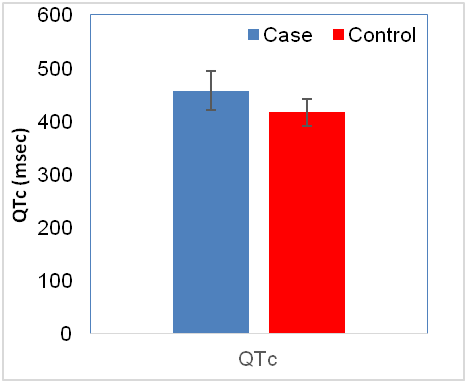
The mean values of ECG parameters were compared between the case and the control groups using independent sample t-test as shown in the Table 1. The results showed a significantly wider QRS (p = 0.011) and longer QT (p = 0.003) and QTc (p = 0.002) in pre-eclamptic pregnancy when compared with control group. There were no significant differences in the P wave duration and PR interval between the two groups. The mean QRS duration in pre-eclamptic women and normotensive pregnant women was found to be 0.10±0.02 and 0.09±0.005 seconds respectively. The mean QT interval was 0.401±0.03 sec in pre-eclamptic women and 0.365±0.014 sec in normotensive pregnant women as shown in Figure 1 and the mean QTc interval was found to be 457.73±37 msec in pre-eclamptic women and 416.47±25.4 msec in normotensive pregnant women as shown in Figure 2 and there was significant difference between the two groups (p=0.002). The pre-eclamptic women had lower heart rate (HR) and higher Sokolow index than normotensive pregnancy but the difference were not statistically significant.
| Variables | Pre-elampsia (Case) | Normotensive (Control) | P-value |
|---|---|---|---|
| HR(bpm) | 77.6±12.85 | 80.87±10.70 | 0.455 |
| P(sec) | 0.082±0.006 | 0.080±0.004 | 0.550 |
| QRS(sec) | 0.10±0.02 | 0.09±0.005 | 0.011* |
| PR(sec) | 0.129±0.01 | 0.137±0.15 | 0.168 |
| QT(sec) | 0.401±0.03 | 0.365±0.014 | 0.003* |
| QTc (msec) | 457.73±37.00 | 416.47±25.40 | 0.002* |
| Sokolow (mm) | 20±0.46 | 18±0.53 | 0.382 |
Discussion
The results of the present study showed a significantly wider QRS, longer QT, prolonged QTc in pre-eclampsia group. There were no significant differences in the P wave duration and PR interval between the two groups. The pre-eclamptic women had lower heart rate and higher Sokolow index than normotensive pregnancy but the differences were not significant. Murphy et al [6] found prolonged QRS complex in women with a history of pre-eclampsia and suggested increased risk of delayed myocardial conduction and arrhythmia in pre-eclamptic women. Raffaelli et al [7] in their investigation compared ECG between pre-eclamptic and normal pregnant women and noted decrease HR, prolonged QT and QTc in pre-eclamptic women and suggested that prolonged QT and QTc in pre-eclamptic women could lead to alteration of the ventricular repolarization.
The mean QRS (sec) of the present study was found to be 0.10±0.02 in pre-eclamptic women and 0.09±0.005 in normotensive pregnant women. However, the value of QRS could not be considered a prolonged QRS as it does not reach ≥ 0.12 sec.
The mean QT (sec) was 0.401±0.03 in pre-eclamptic women and 0.36±0.014 in normotensive pregnant women respectively. However this could not be considered prolonged QT as it falls within normal limits (0.36-0.44 sec)
The mean QTc (msec) was found to be 457.73±37 in pre-eclamptic women and 416.47±25.4 in normotensive pregnant women respectively. The value of QTc in pre-eclamptic women was found to be significantly prolonged.
The QT interval is the time between the start of the Q wave and the end of the T wave in the heart's electrical cycle. The QT interval represents electrical depolarization and repolarization of the ventricles. The QT interval was corrected by HR according to Bazett's formula (QTc (msec) = QT/√RR). Left ventricular hypertrophy (LVH) was assessed by Sokolow-Lyon voltage criteria (S V1+ RV5/V6 > 38mm).
Isezuo et al [8] documented that intrapartum eclamptic patient had significantly higher mean heart rate and higher QTc (470.4 vs 436.3, p<0.05) than the women with uncomplicated pregnancy. QT interval seems to be uneffected by normal pregnancy. Conversely, pregnancies that develop hypertensive disorders seem to be accompanied by changes in ventricular repolarization that may precede clinical symptoms.
Zangeneh et al [9] compared left ventricular mass in pre-eclamptic group and normal pregnant women and observed that pre-eclamptic group had more left ventricular mass but difference were not significant. Melchiorre et al [10] observed that more frequently diastolic dysfunction and increased cardiac work and left ventricular mass indices in pre-eclampsia suggesting that left ventricular remodeling was an adaptive response to maintain myocardial contractility with pre-eclampsia at term. Approximately 20% of patients with pre-eclampsia at term have evident myocardial damage. Diastolic dysfunction usually precedes systolic dysfunction in the evolution of ischemic or hypertensive cardiac diseases and is of prognostic value in the prediction of long-term cardiovascular morbidity. The ECG findings also have significant implications for the acute medical management of pre-eclampsia.
Conclusion
The ECG abnormalities found in the study shows that the pre-eclamptic women are at increased risk of cardiovascular problems. Pre-eclamptic pregnancy has a significant effect on ventricular repolarization, so may lead to an alteration of ventricular repolarization (AVR). AVR is a possible explanation of the increased cardiovascular risk of pre-eclamptic women. Hence, the study shows that electrocardiography can be used to evaluate cardiovascular risk in pre-eclamptic women. Probably the myocardial contractility was conserved in the pre-eclamptic cases and hence there were no statistically significant findings on heart rate and Sokolow’s index.
Source of funding
None
Acknowledgments
None
References
- Duley L. The global impact of pre-eclampsia and eclampsia. Semin Perinatol. 2009 Jun; 33(3):130-7. [Pubmed] [Crossref]
- Konar H. DC Dutta’s Textbook of Obstetrics. 7th ed. New Delhi: Jaypee Brothers Medical Publishers; 2013.
- Sogani S, Varma V, Sarkar PD. Estimation of thyroid hormones levels in preeclamptic pregnant women: an early predictor of the disease. Al Ameen J Med Sci. 2015; 8(4):266-70.
- Baumert M, Seeck A, Faber R, Nalivaiko E, Voss A. Longitudinal changes in QT interval variability and rate adaptation in pregnancies with normal and abnormal uterine perfusion. Hypertens Res. 2010 Jun; 33(6):555-60. [Pubmed] [Crossref]
- Angeli F, Angeli E, Verdecchia P. Novel electrographic patterns for the prediction of hypertensive disorders of pregnancy – from pathophysiology to practical implications. Int J Mol Sci 2015 Aug 7; 16(8):18454-73. [Pubmed] [Crossref]
- Murphy MS, Seaborn GE, Redfearn DP, Smith GN. Reduced heart variability and altered cardiac conduction after preeclampsia. PLoS One. 2015 Sep 25; 10(9):e0138664. [Pubmed] [Crossref]
- Raffaelli R, Prioli MA, Parissone F, Prati D, Carli M, Bergamini C, Cacici G, Balestreri D, Vassanelli C, Franchi M. Pre-eclampsia: evidence of altered ventricular repolarization by standard ECG parameters and QT dispersion. Hypertens Res. 2014 Nov; 37(11):984-8. [Pubmed] [Crossref]
- Isezuo SA, Ekele BA. Eclampsia and the abnormal QTc. West Afr J Med. 2004 Apr-Jun; 23(2):123-7. [Pubmed] [Crossref]
- Zangeneh M, Veisi F, Malekkhosravi S, Rezavand N, Nankali A, Rezaei M, Ghadami MR, Karami A. Electrocardiographic changes in healthy and pre-eclamptic pregnant women. J Kermanshah Univ Med Sci. 2012; 16(4):e78789. [Article in Persian]
- Melchiorre K, Sharma R, Thilaganathan B. Cardiovascular implications in preeclampsia: an overview. Circulation. 2014 Aug 19; 130(8):703-14. [Pubmed] [Crossref]

