Variation in carotid-femoral pulse wave velocity, augmentation pressure and augmentation index during different phases of menstrual cycle
Indicators of arterial stiffness during phases of menstrual cycle
Revised: 2018-11-09
Accepted: 2018-11-28
Online: 2018-11-28
Print: 2018-11-28

Full text
Abstract
Physiological variation of estrogen and progesterone during menstrual cycle is well known. They not only have an effect on blood pressure control, but also seem to have a role in regulating arterial compliance. This study was done to find out whether there are any changes in central arterial parameters during different phases of menstrual cycle. Thirty female subjects in the age group of 18-22 years with normal, regular menstrual cycles participated in this prospective observational study at our teaching hospital. Anthropometric parameters were recorded. Blood pressure in all 4 limbs was recorded using cardiovascular risk analyzer-Periscope™ on Day 3rd to 5th (follicular phase), Day 12th to 14th (ovulation phase), Day 22nd to 24th (luteal phase) of their menstrual cycle. We collected blood samples during these three phases for estimation of estradiol and progesterone by ELISA technique. Analysis of variance and correlation statistics were done using SPSS 17.0 statistical software. No significant statistical changes were observed in systolic blood pressure, diastolic blood pressure, mean arterial pressure, pulse pressure, aortic systolic pressure, aortic diastolic pressure, aortic augmentation pressure, aortic index and pulse wave velocity during the three recorded phases of the menstrual cycle. There are many studies which correlate changes in peripheral artery blood pressure with different phases of menstrual cycle. But there is scarcity in data available which correlates central arterial pressures and arterial stiffness with natural hormonal variations in different phases of menstrual cycle. However, our results show that although there are subtle changes in blood pressure parameters along with estrogen and progesterone levels throughout the menstrual cycle, yet these were not statistically significant.
Keywords
Augmentation index, Carotid femoral pulse wave velocity, Estrogen, Progesterone
Introduction
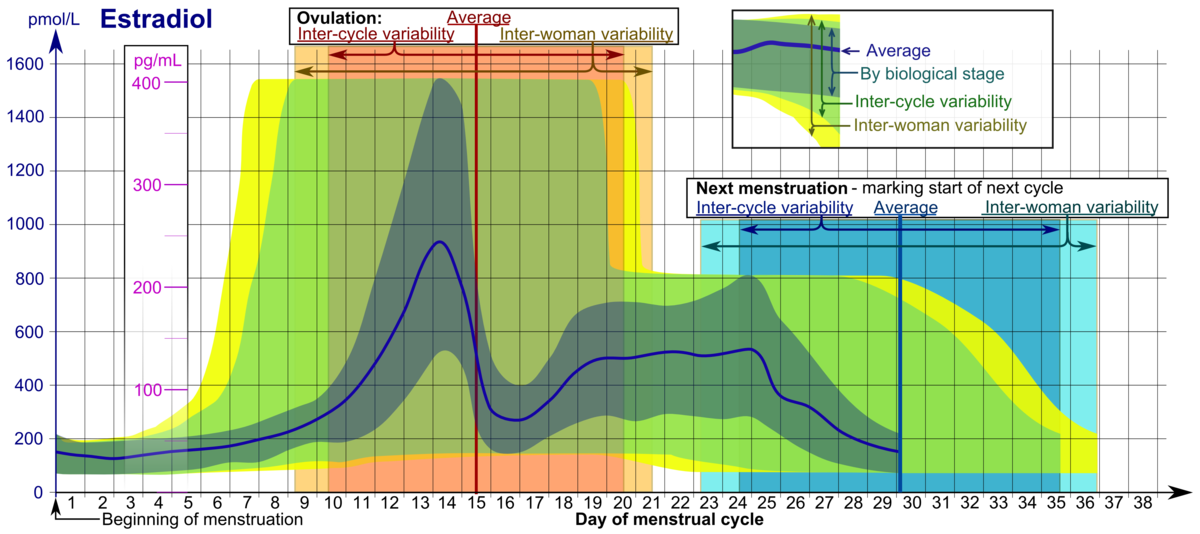
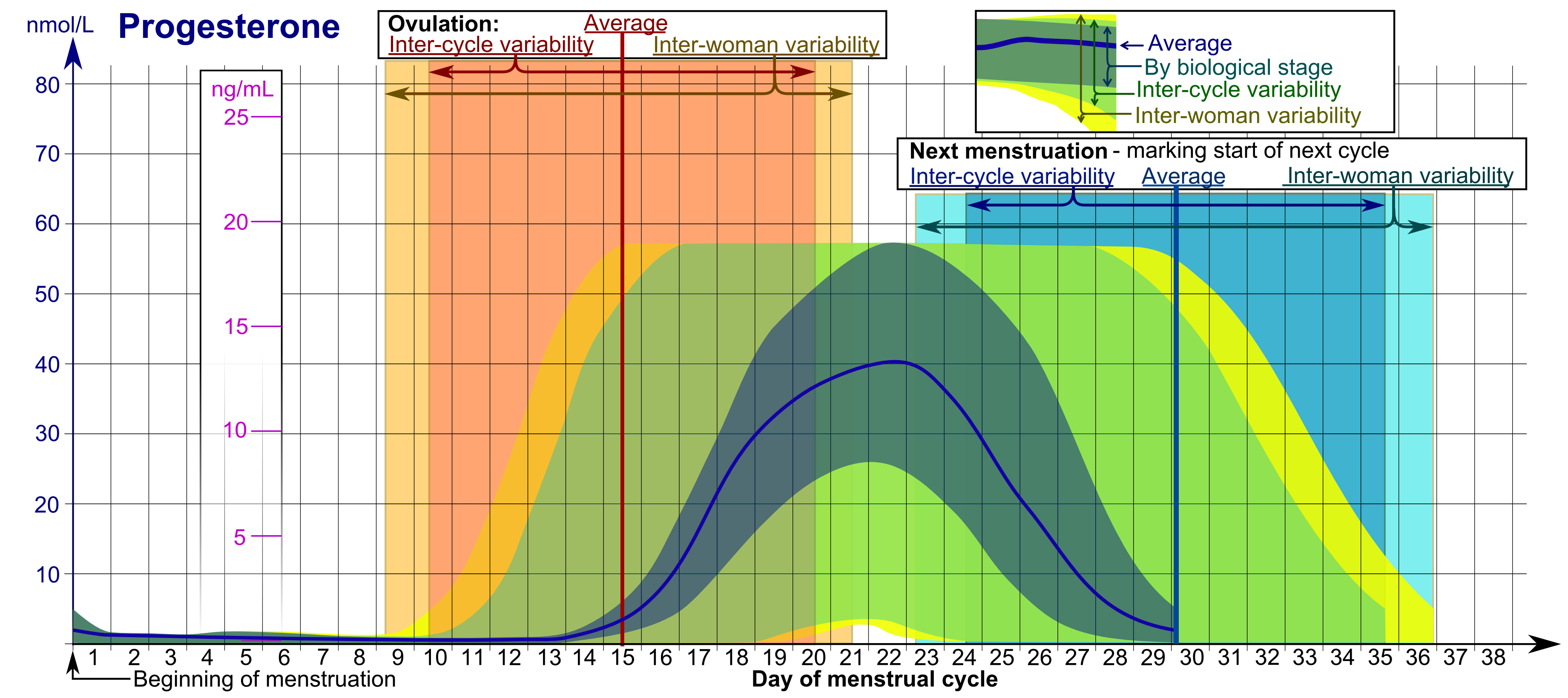
Female sex hormones have diverse physiological effects on different tissues and organs of the body. These sex hormones predominantly produced by the ovaries vary in different phases of menstrual cycle and in different age groups [1]. Pre-menopausal women, when compared to men of the same age, are known to have a less incidence of cardiovascular events. Pregnancy is associated with low blood pressure in spite of presence of sodium retention and increased levels of circulating angiotensin II. The risk of developing cardiovascular disease increases after menopause. This shows that ovarian hormones have a cardio-protective role [2]. Physiological variation of ovarian hormones during menstrual cycle is well known as shown in Figures 1 and 2.
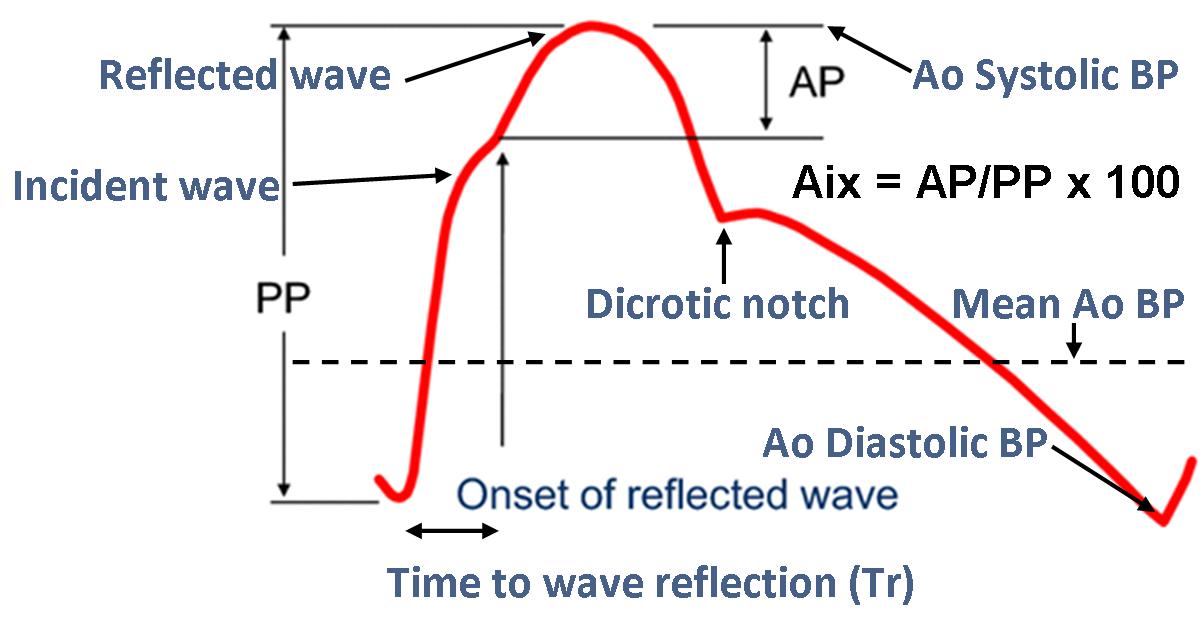
Not only do estrogen and progesterone have an effect on blood pressure control, they also seem to have a role in regulating arterial compliance [3]. Estrogen is predominantly cardio-protective, hence prescribed in menopausal women and those who underwent hysterectomy. Progesterone effects arterial compliance by inducing a state of vasomotor instability and by causing constriction of vessels already primed with estrogen [4,5]. Pulse wave velocity (PWV) is a measure of arterial stiffness. Increase in arterial stiffness is associated with increased incidence of atherosclerosis, hypertension, stroke, and dementia [6]. Studies have reported conflicting results on the variation of pulse wave velocity and arterial compliance with natural hormone fluctuations during menstrual cycle [3,7]. In this study, we hypothesize that the ovarian hormonal variations are significant enough to influence the cardiovascular state including the arterial stiffness, pulse wave velocity and augmentation pressure (Figure 3).
Materials and Methods
This study was conducted in department of Physiology of our medical college during May-June 2017. Sample size included 30 apparently healthy female subjects in the age group of 18-22 years, who are unmarried, nulliparous with regular menstrual cycles in the past 3 months. Those female subjects with history of irregular menstrual cycle, amenorrhea, dysmenorrhea, and menorrhagia, polycystic ovarian disease, anemia, asthma, hypothyroidism, hyperthyroidism or any other chronic disorders were excluded from this study.
Methodology
Informed consent was obtained from the subjects prior to the start of the study. Ethical clearance from Institutional Review Board was taken before the start of this study (Ref. No.: 2017/18/007). Anthropometric parameters like height and weight were measured.
Recording of blood pressure (BP): Blood pressures of the subjects were recorded in supine position in all 4 limbs (Upper limb: brachial artery; Lower limb: Posterior tibial artery) using Cardiovascular risk analyzer-Periscope™ (Genesis Medical System, India). The system generated output gives other cardiovascular parameters including pulse wave velocity (PWV) and augmentation pressure (AP) and augmentation index (Aix). This recording was performed in the afternoon (12:00 pm to 04:00 pm) on 3 days of the menstrual cycle for each subject, i.e. between Day 3-5 (follicular phase), Day 12-14 (ovulation), Day 22-24 (luteal phase). These phases were determined on the basis of previous cycle length and the time of menstruation assuming that the luteal phase duration is 14 days [6].
Estimation of estrogen and progesterone: Blood sample (3 ml) was collected on 3 time points corresponding to the phase of menstrual cycle in serum vacutainers and was sent to the department of Biochemistry of our hospital for estimation of estradiol and progesterone via enzyme-linked immunoassay technique (ELISA) using commercially available kits (Calbiotech, USA).
Statistical analyses
Data obtained was tabulated using Microsoft Excel and imported into SPSS 17.0 statistical software for analysis. Data obtained was analyzed through repeated measures ANOVA using SPSS 17.0 (SPSS Inc, Chicago, USA).
Results
30 apparently young female subjects were enrolled in this study. Some data of 3 participants was missing and hence analysis was performed for 27 subjects. Table 1 shows the demographic values of subjects represented as Mean±Standard deviation (SD).
| Variables | Mean±SD |
|---|---|
| Age (years) | 20.68±0.96 |
| Weight (kg) | 60.86±13.06 |
| Height (cm) | 157.86±4.78 |
| BMI (kg/m2) | 24.34±4.72 |
| Peripheral BP (mm Hg) | Location | Follicular phase | Ovulatory phase | Luteal phase |
|---|---|---|---|---|
| Systolic blood pressure | Right arm | 107.48±6.88 | 107.19±9.48 | 107.11±6.9 |
| Left arm | 107±7.96 | 107.56±9.85 | 106.96±8.06 | |
| Right ankle | 115.56±10.42 | 111.74±9.32 | 114.52±9.51 | |
| Left ankle | 115.81±11.91 | 112.52±9.63 | 114.67±9.59 | |
| Diastolic blood pressure | Right arm | 60.52±5.58 | 60.04±6.26 | 61.22±5.57 |
| Left arm | 61.11±5.56 | 60.11±7.72 | 61.3±5.75 | |
| Right ankle | 59.93±6.62 | 58.15±6.21 | 65.04±5.81 | |
| Left ankle | 62.22±6.88 | 59.41±6.38 | 60.67±6.36 | |
| Pulse pressure | Right arm | 46.96±7.18 | 47.15±7.68 | 45.89±6.01 |
| Left arm | 45.89±6.01 | 47.44±7.44 | 45.67±6.67 | |
| Right ankle | 55.63±7.22 | 53.59±9.12 | 54.48±6.86 | |
| Left ankle | 53.59±10 | 53.11±7.41 | 54±7.82 | |
| Mean arterial pressure | Right arm | 76.17±5.01 | 75.75±6.56 | 76.52±5.34 |
| Left arm | 76.41±5.8 | 75.92±7.73 | 76.52±5.82 | |
| Right ankle | 78.47±7.22 | 76.01±6.02 | 78.19±6.49 | |
| Left ankle | 80.08±7.53 | 77.11±6.77 | 78.66±6.64 |
| Pulse wave velocity (cm/s) | Location | Follicular phase | Ovulatory phase | Luteal phase |
|---|---|---|---|---|
| Heart-brachial | Right arm | 254.62±20.25 | 251.18±19.74 | 248.48±23.86 |
| Left arm | 254.59±18.46 | 248.92±23.84 | 249.67±23.67 | |
| Heart-ankle | Right ankle | 399.48±20.53 | 397.67±17.2 | 397.22±20.81 |
| Left ankle | 400±21.94 | 394.37±22.34 | 399.70±19.54 | |
| Carotid femoral | 596.17±72.44 | 595.79±63.28 | 609.77±70.83 |
| Parameter | Follicular phase | Ovulatory phase | Luteal phase |
|---|---|---|---|
| Aortic SBP (mm Hg) | 87.52±6.90 | 87.78±8.74 | 87.67±6.83 |
| Aortic DBP (mm Hg) | 61±4.82 | 60.37±6.15 | 61.37±4.88 |
| Aortic pulse pressure (mm Hg) | 26.15±4.91 | 27±5.45 | 25.96±4.69 |
| Aortic MAP (mm Hg) | 69.72±5.08 | 69.37±6.61 | 70.02±5.12 |
| Augmentation pressure (mm Hg) | 0.22±1.69 | 0.59±1.65 | 0.37±1.55 |
| Augmentation index (%) | -0.07±0.0 | 0.85±6.90 | 0.37±7.16 |
The peripheral arterial parameters did not show any statistically significant result with repeated measures ANOVA. These include right arm SBP [F(2) = 0.646, p = 0.528]; right arm DBP [F(2) = 0.875, p = 0.423]; right arm pulse pressure [F(2) = 0.107, p = 0.898]; right arm MAP [F(2) = 1.125, p = 0.333]; left arm SBP [F(2) = 0.342, p = 0.712]; left arm DBP [F(2) = 0.618, p = 0.543]; left arm MAP [F(2) = 0.639, p = 0.532]; right ankle SBP [F(2) = 0.325, p = 0.724]; right ankle DBP [F(2) = 0.843, p = 436]; right ankle PP [F(2) = 0.209, p = 0.812]; right ankle MAP [F(2) = 0.679, p = 0.512]; left ankle SBP [F(2) = 0.751, p = 0.477]; left ankle DBP [F(2) = 2.071, p = 0.137]; left ankle MAP [F(2) = 1.918, p = 0.158].
A repeated measures ANOVA with Greenhouse-Geisser correction determined that mean left arm pulse pressure and mean left ankle pulse pressure also did not differ significantly between the 3 menstrual phases [F(1.58) = 0.099, p = 0.862; F(1.332) = 0.152, p = 0.77 respectively].
The central arterial parameters also did not show any statistically significant result. These include aortic systolic pressure [F(2) = 0.031, p = 0.97]; aortic diastolic pressure [F(2) = 0.662, p = 0.52]; aortic pulse pressure [F(2) = 0.813, p = 0.449]; aortic MAP [F(2) = 0.312, p = 0.733]; aortic augmentation pressure [F(2) = 0.769, p = 0.469]; augmentation index [F(2) = 0.27, p = 0.764].
| Hormone | Follicular phase | Ovulatory phase | Luteal phase |
|---|---|---|---|
| Estrogen (pg/ml) | 33.21±5.82 | 31.41±3.55 | 32.17±3.22 |
| Progesterone (ng/ml) | 42.79±4.91 | 41.97±5.75 | 41.28±4.11 |
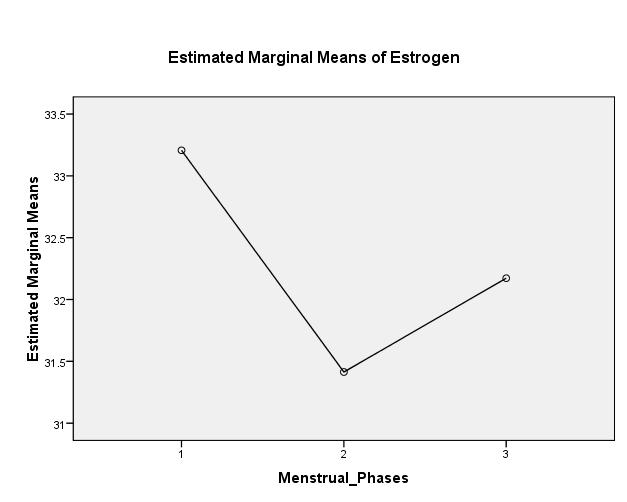
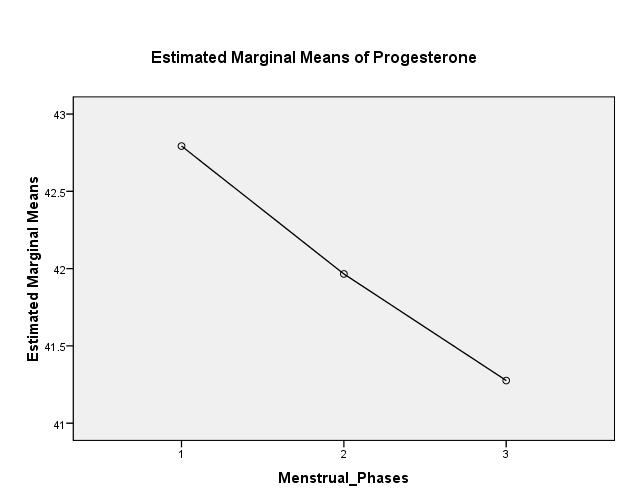
Estrogen [F(1.351) = 2.201, p = 0.139] and progesterone [F(2) = 1.48, p = 0.236] did not show any significant variation during the 3 phases (Table 5; Figure 4 and 5 respectively).
Discussion
This study was conducted with the aim of knowing the differences in pulse wave velocity, augmentation pressure and augmentation index in different phases of menstruation. The findings of current study did not show any statistically significant difference in estrogen and progesterone levels. This may be attributed to inter-cycle and inter-subject variability as presented by Häggström [1].
The SBP and DBP did not vary significantly between follicular, ovulatory and luteal phases. This finding is in conformity with our earlier study [5] and also with a study done by Minson et al [8].
The current study did not show any significant difference pertaining to aortic pressure parameters during various phases of ovulatory cycle. Aortic systolic, diastolic, MAP, PP, AP and Aix changes were very minimal and statistically not significant. Aortic root pressure is dependent on arterial distensibility which in turn is influenced by the changes in serum estradiol levels. As in this study there was no significant variation seen in estrogen levels, changes in aortic parameters were also insignificant. Our findings are in contrast to those seen in studies done by Chapman et al [9] and Hayashi et al [3].
The PWV also did not vary with phases of menstrual cycle in this study which is an index of arterial stiffness or distensibility. Our study did not reveal any obvious fluctuations in the hormonal levels therefore our findings did not correlate with the study of Giannattasio et al [10].
Since age of the subjects was within a narrow range, it was not possible to correlate the variation in estrogen levels with age as was shown in a study done by Clarkson et al [11]. The hormonal variations between the three menstrual phases were minimal and therefore no significant variation could be observed in central and peripheral arterial pressure parameters with the levels of estrogen and progesterone measured during follicular, ovulatory and luteal phases of menstrual cycle. This finding is in contrast to a study done by Macedo et al which found a reduction in central aortic blood pressure, mean arterial blood pressure, aortic stiffness and augmentation index in normal pregnancy. Most significant changes were observed during mid pregnancy; the beneficial effect of female sex hormones may be attributable to this [12].
Conclusion
There are many studies which correlate changes in peripheral artery blood pressure with different phases of menstrual cycle. But there is scarcity in data available which correlates central arterial pressures and arterial stiffness with natural hormonal variations in different phases of menstrual cycle. Hence this study made an attempt to record the central arterial pressures and correlate the indices of arterial stiffness like pulse wave velocity and augmentation pressure with hormonal variations during menstrual cycle. This study concludes that there is no statistically significant variation in peripheral and central arterial parameters with hormonal variations during regular menstrual cycle. This could be attributed to minimal changes in hormonal levels during the 3 phases of menstrual cycle, the age group of the subjects which was of a narrow range and the time of collection of blood samples.
Limitations of this study: Since the sample size was less, we couldn’t find any statistically significant relation between central and peripheral arterial parameters with hormonal fluctuations during menstrual cycle.
Source of funding
This study was partly supported by ICMR-Short Term Studentship awarded to Ms. Nudrat Kahkashan (ICMR STS Reference ID: 2017-06742) and ICMR Extramural research grant (IRIS ID: 2012-0836; Principal Investigator: Dr. Mohammed Abdul Hannan Hazari).
Acknowledgments
None
References
- Häggström M. Reference ranges for estradiol, progesterone, luteinizing hormone and follicle-stimulating hormone during the menstrual cycle. WikiJournal of Medicine. 2014; 1:1. [Crossref]
- Barbagallo M, Dominguez LJ, Licata G, Shan J, Bing L, Karpinski E, Pang PK, Resnick LM. Vascular effects of progesterone: Role of cellular calcium regulation. Hypertension. 2001 Jan; 37(1):142-7. [Pubmed] [Crossref]
- Hayashi K, Miyachi M, Seno N, Takahashi K, Yamazaki K, Sugawara J, Yokoi T, Onodera S, Mesaki N. Variations in carotid arterial compliance during the menstrual cycle in young women. Exp Physiol. 2006 Mar; 91(2):465-72. [Pubmed] [Crossref]
- Rosano GM, Sarias C, Zoncu S, Mercuro G. The relative effect of progesterone and progestins in hormone replacement therapy. Hum Reprod. 2000 Jun; 15 Suppl 1:60-73. [Pubmed]
- Arifuddin MS, Hazari MA, Reddy BR. Blood pressure variations during different phases of menstrual cycle. International Journal of Science and Nature 2012; 3:551-4.
- Madhura M, Sandhya TA. Effect of different phases of menstrual cycle on reflection index, stiffness index and pulse wave velocity in healthy subjects. J Clin Diagn Res. 2014 Sep; 8(9):BC01-4. [Pubmed] [Crossref]
- Williams MR, Westerman RA, Kingwell BA, Paige J, Blombery PA, Sudhir K, Komesaroff PA. Variations in endothelial function and arterial compliance during the menstrual cycle. J Clin Endocrinol Metab. 2001 Nov; 86(11):5389-95. [Pubmed] [Crossref]
- Minson CT, Halliwill JR, Young TM, Joyner MJ. Influence of the menstrual cycle on sympathetic activity, baroreflex sensitivity, and vascular transduction in young women. Circulation. 2000 Feb 29; 101(8):862-8. [Pubmed] [Crossref]
- Chapman AB, Zamudio S, Woodmansee W, Merouani A, Osorio F, Johnson A, Moore LG, Dahms T, Coffin C, Abraham WT, Schrier RW. Systemic and renal hemodynamic changes in the luteal phase of the menstrual cycle mimic early pregnancy. Am J Physiol. 1997 Nov; 273(5 Pt 2):F777-82. [Pubmed] [Crossref]
- Giannattasio C, Failla M, Grappiolo A, Stella ML, Bo AD, Colombo M, Mancia G. Fluctuations of radial artery distensibility throughout the menstrual cycle. Arterioscler Thromb Vasc Biol. 1999; 19(8):1925-9. [Pubmed] [Crossref]
- Clarkson TB. Estrogen effects on arteries vary with stage of reproductive life and extent of subclinical atherosclerosis progression. Menopause. 2007 May-Jun; 14(3 Pt 1):373-84. [Pubmed] [Crossref]
- Macedo ML, Luminoso D, Savvidou MD, McEniery CM, Nicolaides KH. Maternal wave reflections and arterial stiffness in normal pregnancy as assessed by applanation tonometry. Hypertension. 2008 Apr; 51(4):1047-51. [Pubmed] [Crossref]

